Introduction
- The U.S. health care system faces significant challenges that are taking a toll on even the most dedicated medical professionals. From administrative burden to staffing shortages and reimbursement challenges, physicians across the country are experiencing long hours and high levels of stress and burnout. Despite these challenges, physicians are increasingly tasked with achieving more with less, including diminished pay.
- With over 80% of U.S. physicians as members, Doximity is the leading digital platform for U.S. medical professionals and maintains one of the largest physician compensation data sets in the U.S. Doximity found that after several years of modest or declining growth, the average pay for doctors increased nearly 6% in 2023, rebounding from a decline of 2.4% in 2022. While this increase appears to be a step in the right direction, inflationary pressures continue to impact physicians’ real income. According to the American Medical Association, when adjusted for inflation, Medicare physician payment has dropped 26% since 2001.1
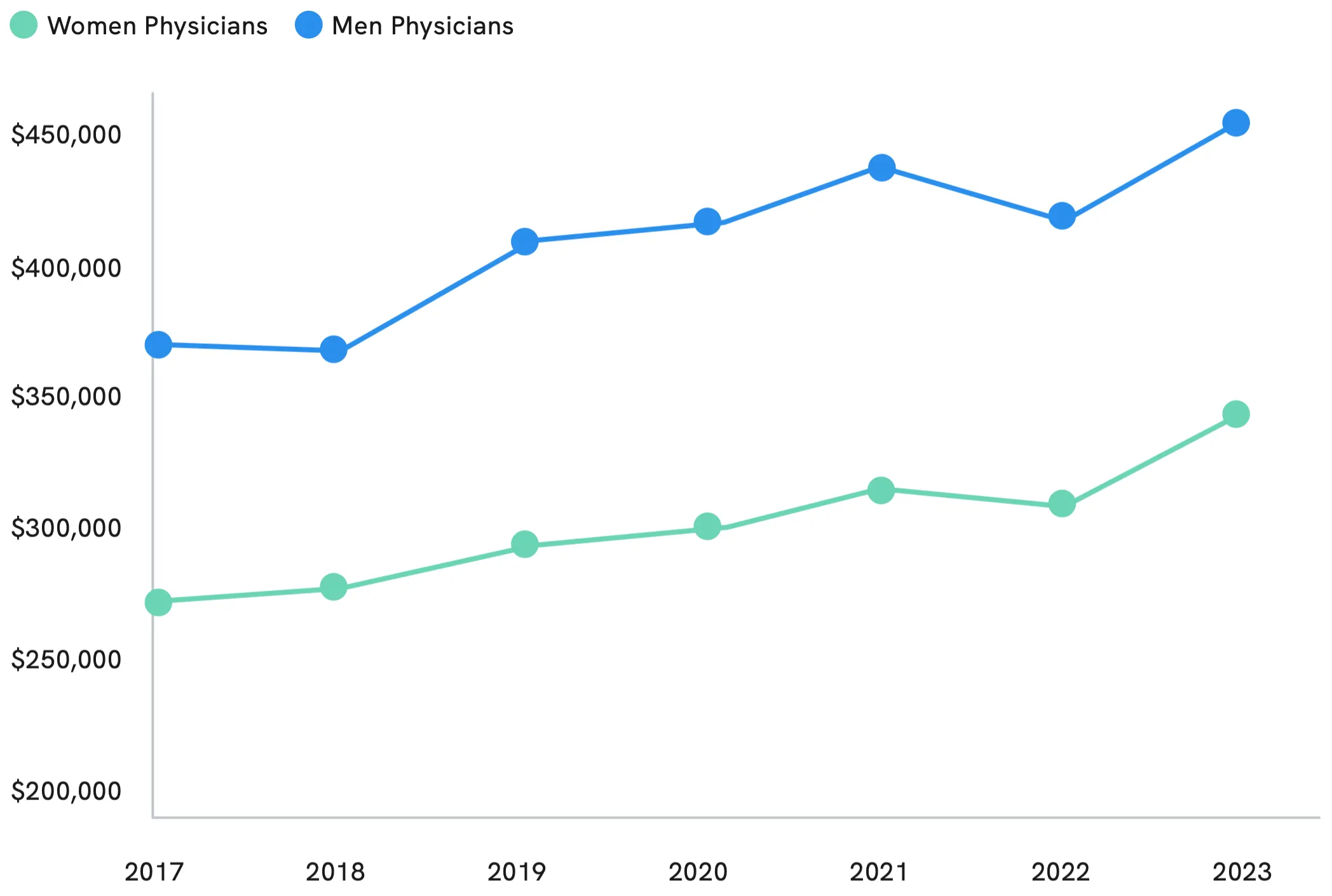
- Another physician compensation challenge that appears to be making modest progress is the gender wage gap, which declined to 23% in 2023, compared to 26% in 2022 and 28% in 2021. Still, the gender pay gap remains substantial, and awareness among many physicians appears to be lacking. Nearly half of physicians surveyed (48%) are either unsure about the gender pay gap or do not believe there is a disparity, and this number is even higher among men.
- Overall, the majority of physicians do not believe their pay matches the level of effort and expertise required in their role, and negotiation attempts are often unsuccessful or nonexistent. Heavy workloads and high administrative burden appear to be so problematic that many physicians are either considering accepting lower compensation for more work-life balance or leaving clinical practice altogether.
- As physician burnout and workforce shortages persist, physicians are concerned about the future of patient care. From longer wait times to delayed diagnosis and intervention, physicians are already witnessing adverse effects on patients. Looking ahead, 86% of physicians are concerned about the U.S. health care system’s ability to care for an aging population.
- The goal of this report is to provide key insights into physician compensation trends and critical challenges facing the physician workforce. By increasing awareness, Doximity aims to help doctors advocate for themselves and make better-informed career decisions. This year's compensation data draws from nearly 150,000 survey responses over five years, including responses from more than 33,000 U.S. physicians in 2023 alone.
Metro Areas


Compensation by Metro Area
Average Physician Compensation Up Nearly 6%
Between 2022 and 2023, the average compensation for U.S. physicians increased nearly 6% (5.9%), rebounding from a slight decline of 2.4% in the previous year. Physicians in the San Jose metropolitan area experienced one of the most significant surges in compensation, with an annual growth rate of 13.5%. This sizable increase propelled San Jose from being the fourth-highest metro area in average physician compensation in 2022 to claiming the number-one spot in 2023.
Notably, all ten of the metropolitan areas with the lowest average physician compensation in 2023 saw growth last year, with growth rates exceeding 10% in Baltimore, Providence, and Virginia Beach.
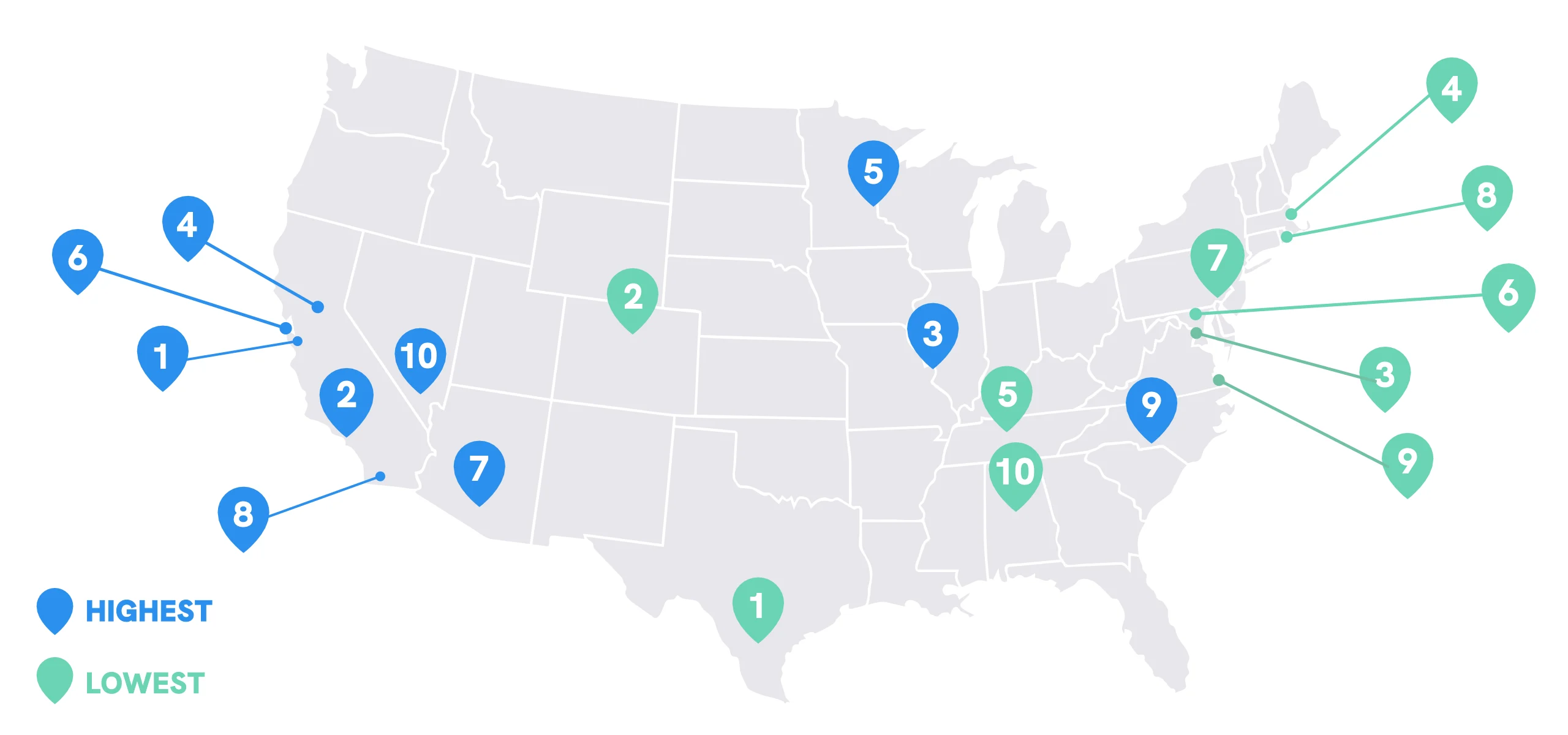
Metro Areas with the HIGHEST Compensation
| Metro Area | Average Compensation |
|---|---|
| 1. San Jose, CA | $474,977 |
| 2. Los Angeles, CA | $448,121 |
| 3. St. Louis, MO | $442,576 |
| 4. Sacramento, CA | $440,004 |
| 5. Minneapolis, MN | $438,756 |
| 6. San Francisco, CA | $437,628 |
| 7. Phoenix, AZ | $436,837 |
| 8. San Diego, CA | $430,187 |
| 9. Charlotte, NC | $429,566 |
| 10. Las Vegas, NV | $426,727 |
Metro Areas with the LOWEST Compensation
| Metro Area | Average Compensation |
|---|---|
| 1. San Antonio, TX | $371,073 |
| 2. Denver, CO | $371,215 |
| 3. Washington, DC | $371,495 |
| 4. Boston, MA | $378,273 |
| 5. Nashville, TN | $380,533 |
| 6. Baltimore, MD | $382,837 |
| 7. Philadelphia, PA | $387,254 |
| 8. Providence, RI | $390,096 |
| 9. Virginia Beach, VA | $390,604 |
| 10. Birmingham, AL | $391,290 |
Cost of Living by Metro Area
Physician Compensation Strongest in St. Louis When Adjusted for Cost of Living
While physicians overall saw an increase in average compensation last year, cost of living remains a crucial factor impacting a physician’s real income. Notably, seven out of the top 10 metro areas with the highest adjusted compensation in 2023 also appeared on the top 10 list in 2022. Joining the top 10 list this year are Las Vegas, New Orleans, and Jacksonville, boasting favorable cost-of-living profiles and annual physician compensation growth rates surpassing the national average.
Consistent with prior years, all cities with the lowest adjusted compensation in 2023 are located on either the East or West Coast, with the exception of Denver. These cities also appeared on the lowest adjusted compensation lists in 2022 and 2021.
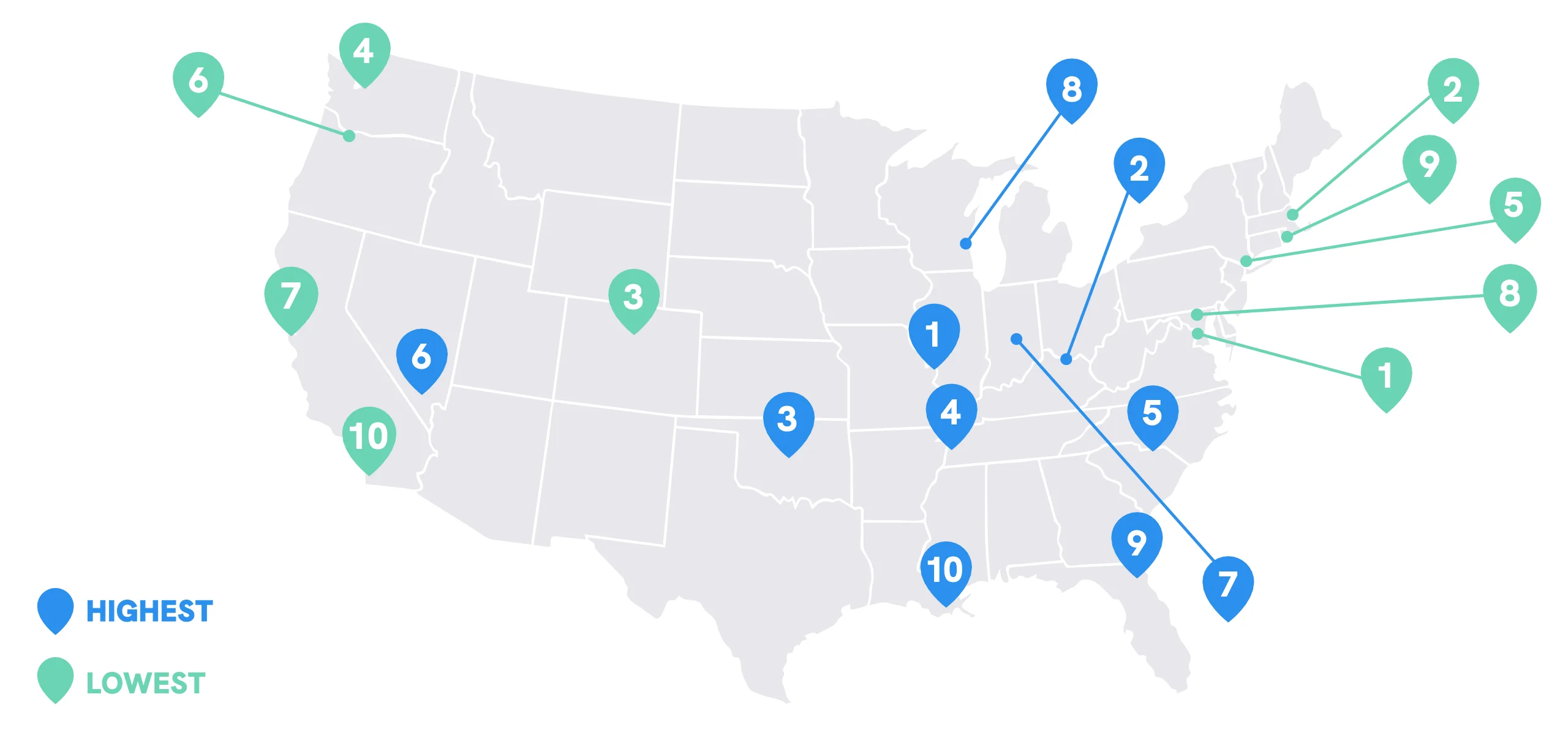
HIGHEST Compensation Adjusted for Cost of Living
| Metro Area |
|---|
| 1. St. Louis, MO |
| 2. Louisville, KY |
| 3. Oklahoma City, OK |
| 4. Memphis, TN |
| 5. Charlotte, NC |
| 6. Las Vegas, NV |
| 7. Indianapolis, IN |
| 8. Milwaukee, WI |
| 9. Jacksonville, FL |
| 10. New Orleans, LA |
LOWEST Compensation Adjusted for Cost of Living
| Metro Area |
|---|
| 1. Washington, DC |
| 2. Boston, MA |
| 3. Denver, CO |
| 4. Seattle, WA |
| 5. New York, NY |
| 6. Portland, OR |
| 7. San Francisco, CA |
| 8. Baltimore, MD |
| 9. Providence, RI |
| 10. San Diego, CA |
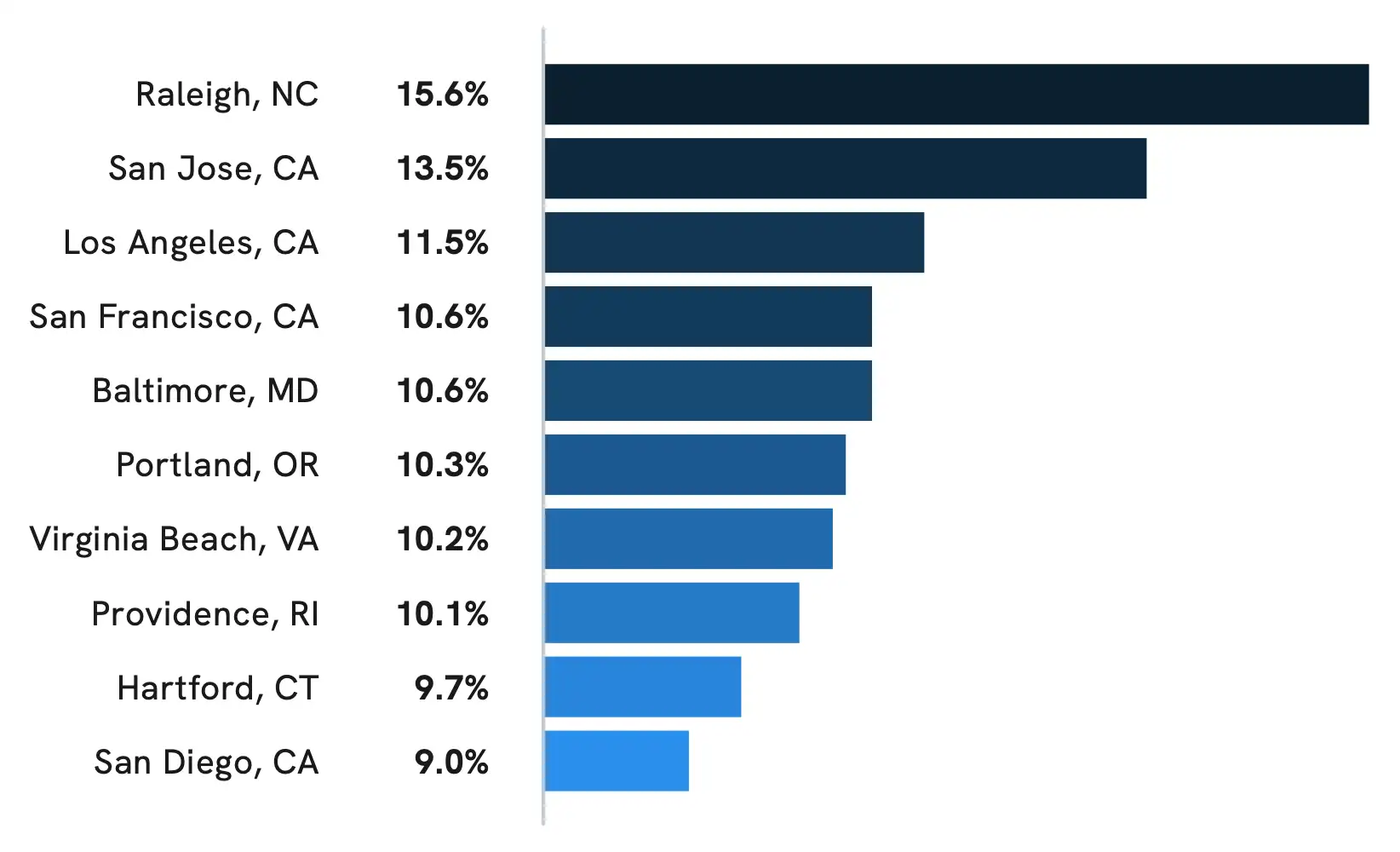
Physician Compensation Growth by Metro Area
Eight Metro Areas Deliver Double-Digit Growth
In 2023, eight of the 50 metropolitan areas studied saw average physician compensation increase by more than 10%, with 30 metropolitan areas experiencing growth rates surpassing 6%. This is a considerable difference from the more stagnant physician compensation growth rates observed in 2022, when most of the top 10 metro areas saw growth rates below 3%, with only one area exceeding 6%.
While this physician compensation growth appears strong, significant economic factors, such as Medicare physician payment cuts in the wake of 40-year high inflation rates, are likely to continue impacting physicians’ real income.1,2
Specialty & Practice Setting


Compensation by Specialty
Adult Surgical and Procedural Specialties Continue to Lead in Average Compensation
Consistent with prior years, the 20 specialties with the HIGHEST average annual compensation tend to be surgical and procedural specialties treating adult patients.

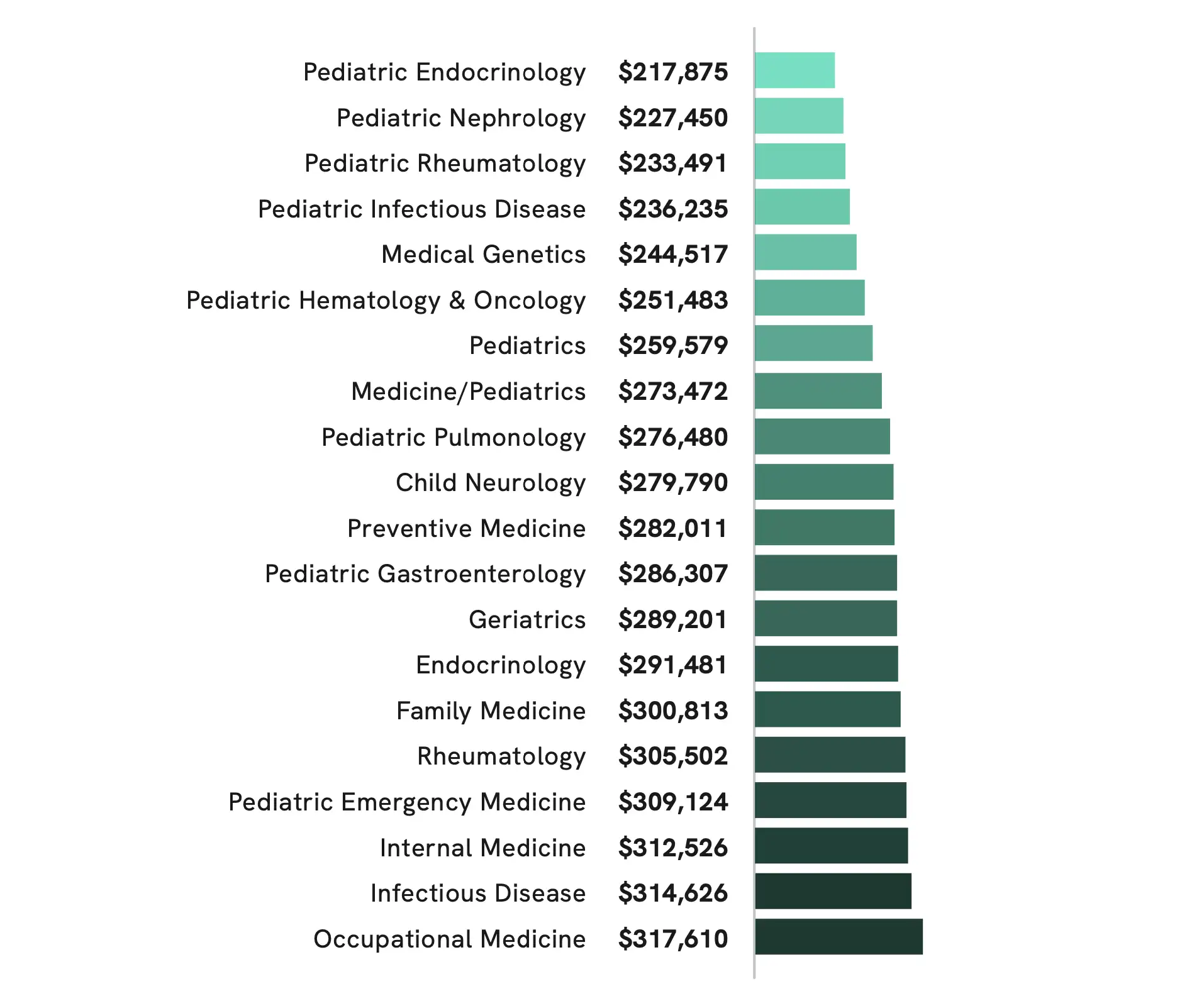
The 20 specialties with the LOWEST average annual compensation tend to be pediatric and primary care specialties
Compensation Growth by Specialty
Hematologists, Family Medicine Physicians Report Double-Digit Growth in 2023
In 2022, physician compensation was flat or down across the majority of all specialties studied. However, in 2023, most specialties experienced positive growth, with the top 10 seeing annual growth rates exceeding 7%.
Hematology and Family Medicine claimed the top two spots in 2023, with double-digit percentage growth compared to 2022. Still, both of these specialties, along with the majority of the 10 specialties with the strongest growth rates in 2023, experienced marginal declines in average annual compensation in 2022.
Only three specialties on this year’s top 10 list—Plastic Surgery, Oral & Maxillofacial Surgery, and Pediatric Emergency Medicine—also showed positive growth rates in 2022.
The top 10 specialties with the LARGEST increase in average annual compensation
| Specialty | Compensation Growth | Average Compensation |
|---|---|---|
| Hematology | 12.4% | $392,260 |
| Family Medicine | 10.2% | $300,813 |
| Infectious Disease | 9.0% | $314,626 |
| Plastic Surgery | 8.5% | $619,812 |
| Occupational Medicine | 8.5% | $317,610 |
| Oral & Maxillofacial Surgery | 8.4% | $603,623 |
| Nephrology | 7.7% | $365,323 |
| Pediatric Emergency Medicine | 7.5% | $309,124 |
| Oncology | 7.3% | $479,754 |
| Psychiatry | 7.2% | $332,976 |
Compensation by Practice Setting
Single Specialty, Multi-Specialty Groups and Solo Practices Continue to Lead
Consistent with prior years, physician compensation showed significant variation depending on the practice setting, with single specialty groups, multi-specialty groups, and solo practices ranking highest in average annual compensation after adjusting for specialty. It is worth noting that physician compensation across all settings saw some positive growth in 2023, with the majority experiencing annual growth rates exceeding 5%. In contrast, in 2022, average physician compensation was relatively flat or slightly down across all practice settings.
Physician Compensation by Practice Setting
| Employment Setting | Average Compensation |
|---|---|
| Single Specialty Group | $461,368 |
| Multi-Specialty Group | $447,546 |
| Solo Practice | $443,274 |
| Health System / IDN / ACO | $427,827 |
| Hospital | $422,146 |
| Health Maintenance Organization | $405,902 |
| Industry | $384,195 |
| Academic | $365,092 |
| Hospital/System - Ambulatory | $357,181 |
| Government | $292,408 |
| Urgent Care Center/ Chain | $288,514 |
Gender Pay Gap


Physician Gender Pay Gap
Gender Pay Gap Remains Pronounced at 23%
In 2023, the gender pay gap for physicians decreased to 23%, marking a slight improvement from the 26% reported in 2022. Despite this progress, the pay gap remains significant, with women physicians earning nearly $102,000 less than men physicians, on average, after controlling for specialty, location, and years of experience.
Although a 3% decrease in the gender pay gap could be a positive sign, it is important to consider it in the context of the overall compensation trends observed in 2023. Notably, this reduction occurred at only half the rate of the 6% increase in average physician compensation during the same period.
An analysis of our physician compensation data from 2014-2019 estimated that over the course of a career, men physicians make over $2 million more than women physicians.3
Physician Average Annual Compensation
Physician Gender Pay Gap by Specialty
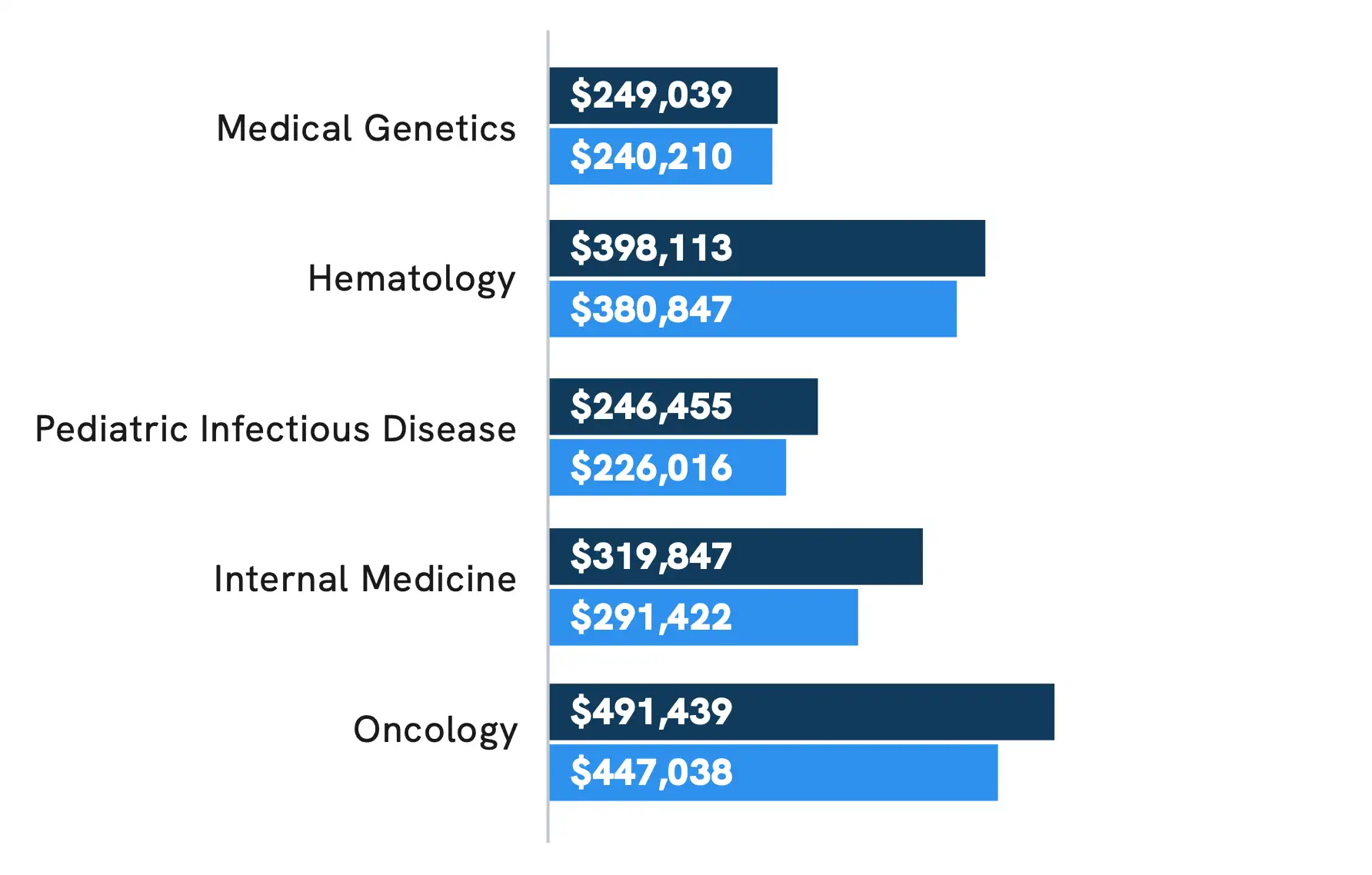
Men Report Higher Compensation Than Women in All Specialties
Consistent with prior years, in 2023, no medical specialties had equal or higher earnings for women physicians compared to men physicians. All specialties had gender pay gaps exceeding 8%, with the exception of three specialties: Medical Genetics (3.5%), Hematology (4.3%), and Occupational Medicine (6.5%).
One positive trend worth noting is the number of specialties narrowing their gender pay gaps to less than 10%. Last year, 12 specialties had pay gaps under 10%, compared to only two specialties in 2022 and one specialty in 2021. Looking ahead, maintaining and advancing this trend will require ongoing commitment, collaboration, and transparency across the medical community.
Medical Specialties with the LARGEST Pay Gaps Between MEN and WOMEN in 2023
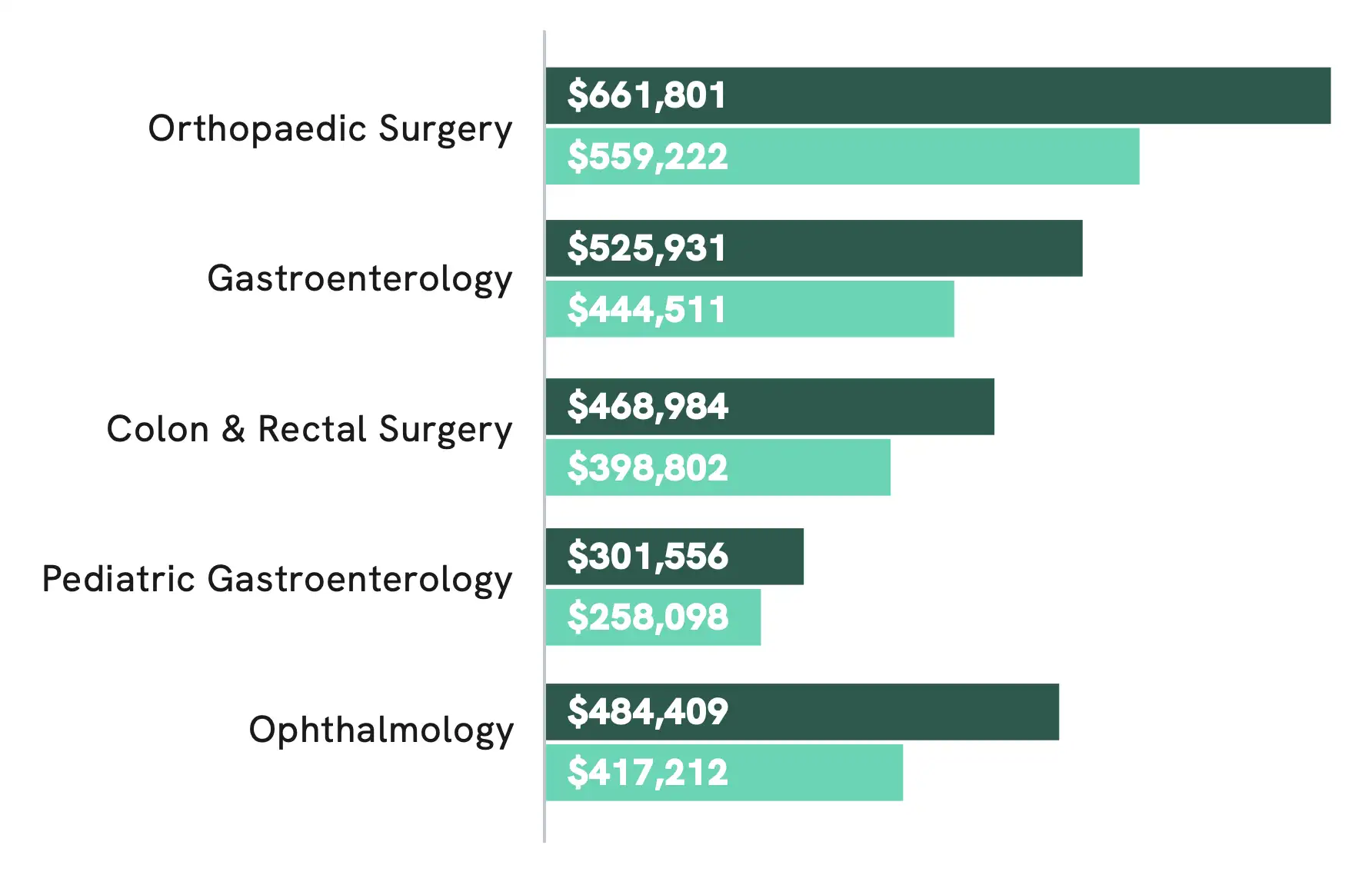
Medical Specialties with the SMALLEST Pay Gaps Between MEN and WOMEN in 2023
Physician Beliefs About Gender Pay Gap
Women Physicians Significantly More Likely to Say There Is a Disparity
One of the most critical steps to closing the physician gender pay gap is raising awareness of its existence. In a survey of over 1,000 physicians, conducted in February and March 2024, about half (nearly 52%) said they believe there is a disparity in how men and women physicians are compensated. However, gender appears to impact this belief. While nearly 75% of women physicians surveyed believe there is a pay disparity, fewer than 30% of men physicians also believe this is true.
Do you believe there is a disparity in how men and women physicians are compensated?
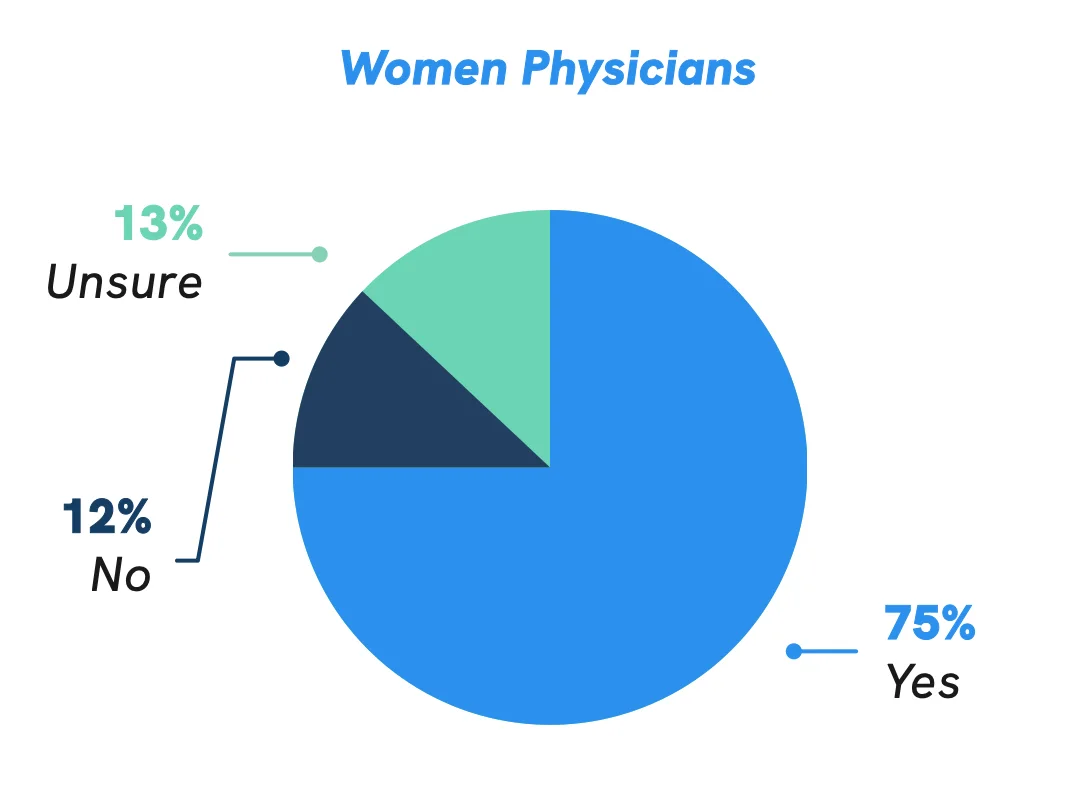
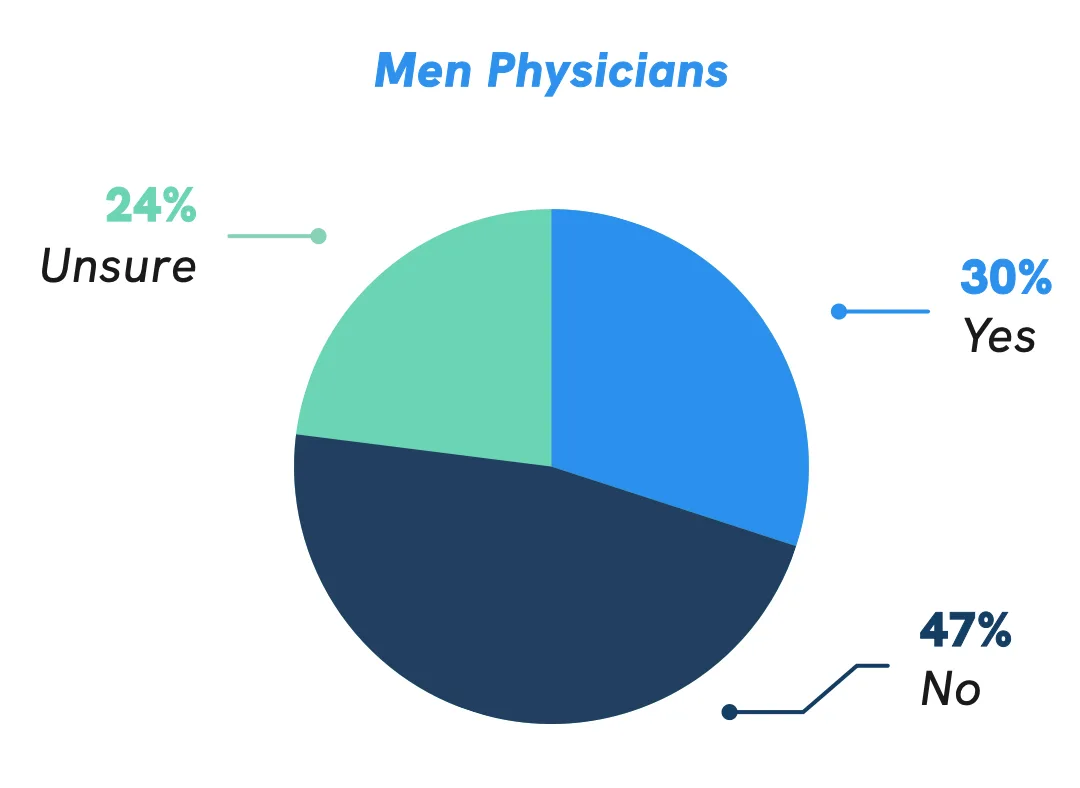
*Due to rounding, numbers may not sum to 100%.
Career & Compensation Satisfaction


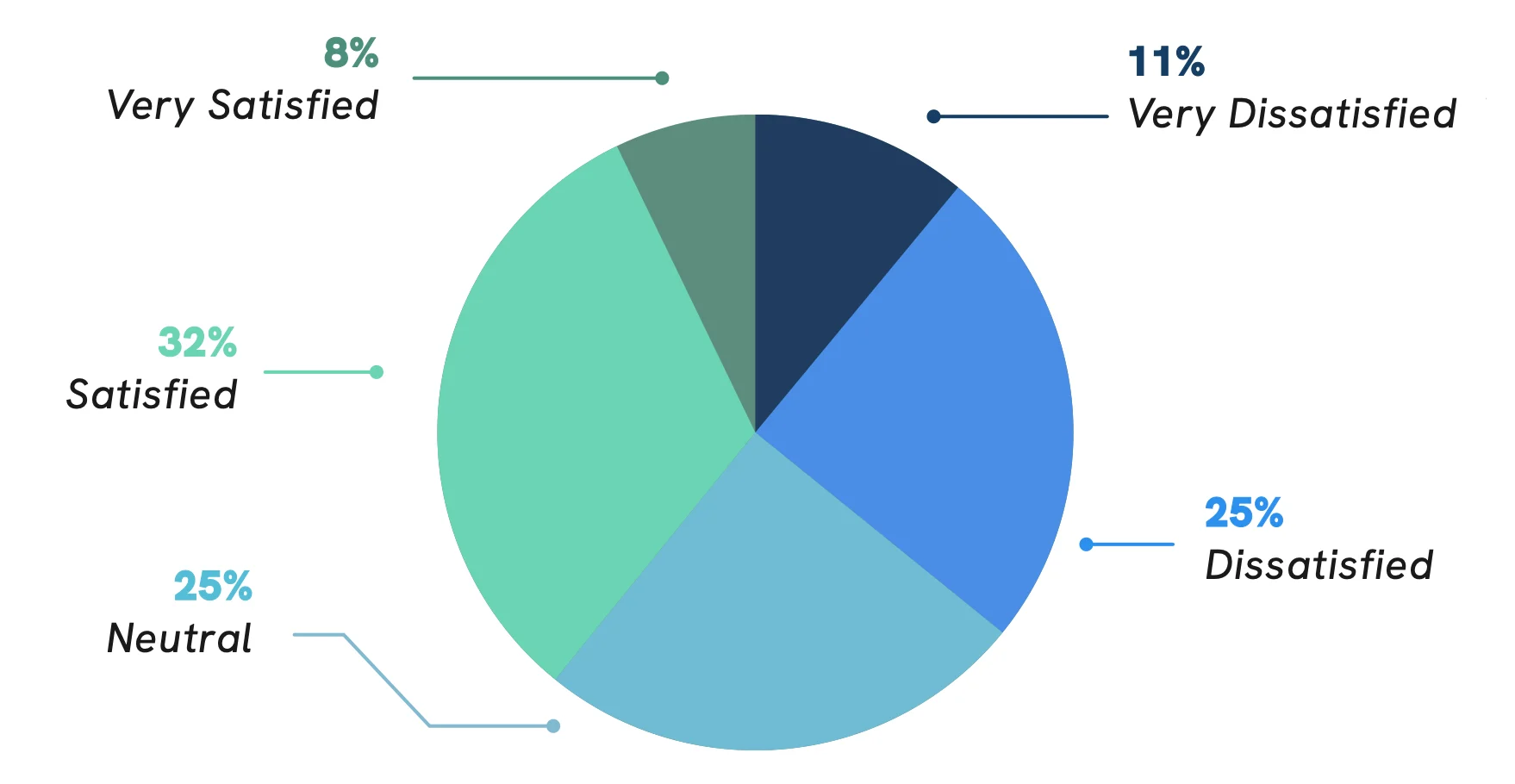
Salary and Compensation Satisfaction
Many Physicians Unsatisfied, Underwhelmed with Their Compensation
In February and March 2024, Doximity surveyed over 1,000 physicians regarding their career and compensation satisfaction. While the gender wage gap remains significant, men and women physicians reported similar levels of satisfaction, or dissatisfaction, with their compensation. More than 39% of women physicians said they are satisfied or very satisfied with their compensation, compared with about 40% of men. Similarly, 35% of both men and women physicians said they are dissatisfied or very dissatisfied with their compensation.
Overall, fewer than one-third (31%) of all physicians surveyed said they believe their compensation reflects the level of expertise and effort required in their role.

How satisfied are you with your current salary and compensation package?
Do you believe that your compensation reflects the level of expertise and effort required in your role?
*Due to rounding, numbers may not sum to 100%.
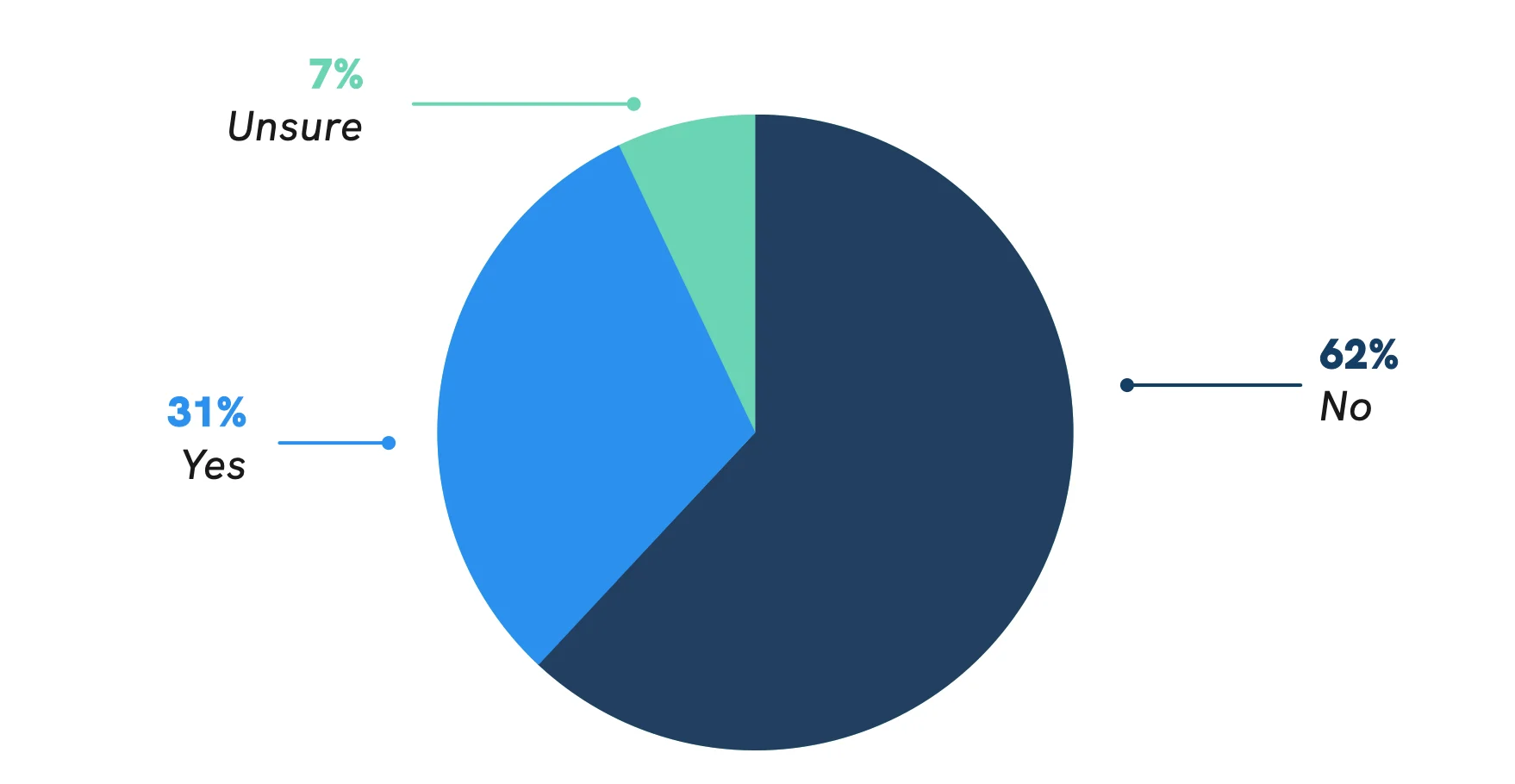
Compensation Negotiation Trends and Challenges
Physician Negotiation Efforts Often Unsuccessful or Nonexistent
While many physicians do not believe their compensation reflects the level of effort and expertise required in their role, the majority of physicians surveyed (63%) either have been unsuccessful in their negotiation attempts or have not tried negotiating at all. Only 5% of physicians surveyed said they have negotiated and were successful in their negotiations.
One possible explanation for this trend is that physicians spend decades focused on education and training, often entering the paid workforce relatively late compared to other professionals. Given their focus on learning, service, and patient care, many physicians might not be aware of their economic value and ability to negotiate, and when they do, may lack direct experience navigating these types of conversations.
Have you previously negotiated (or renegotiated) your compensation package?
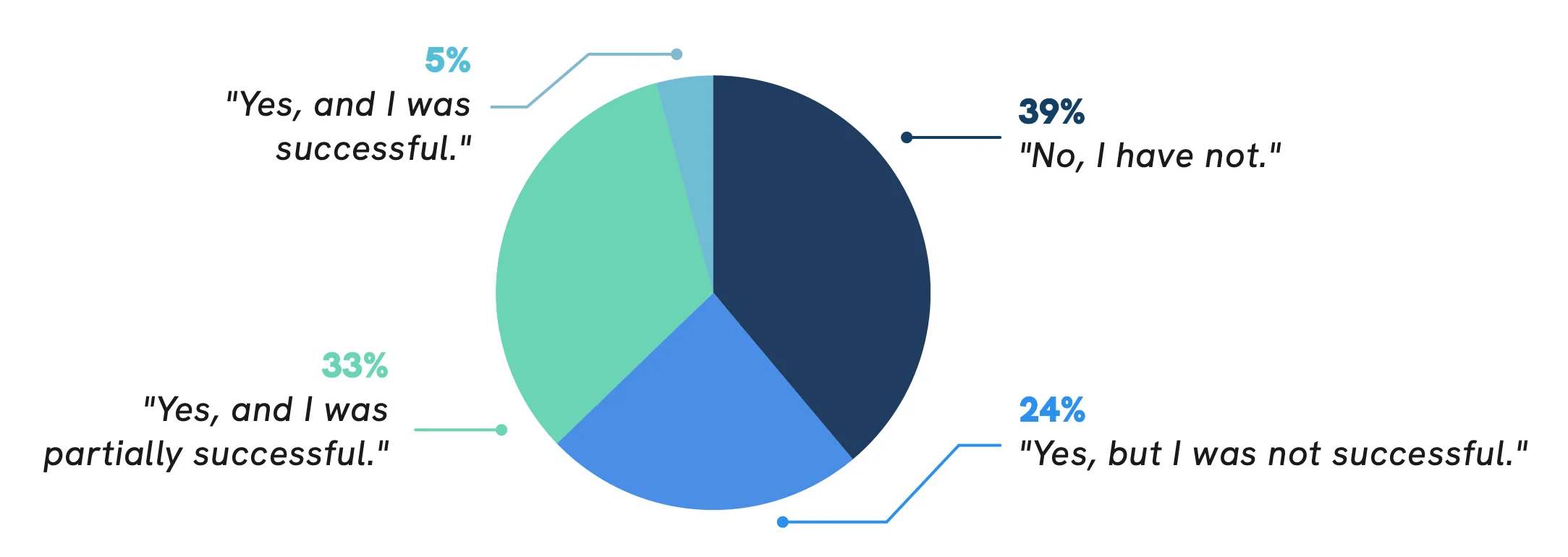
*Due to rounding, numbers may not sum to 100%.
Importance of Autonomy and Work-Life Balance
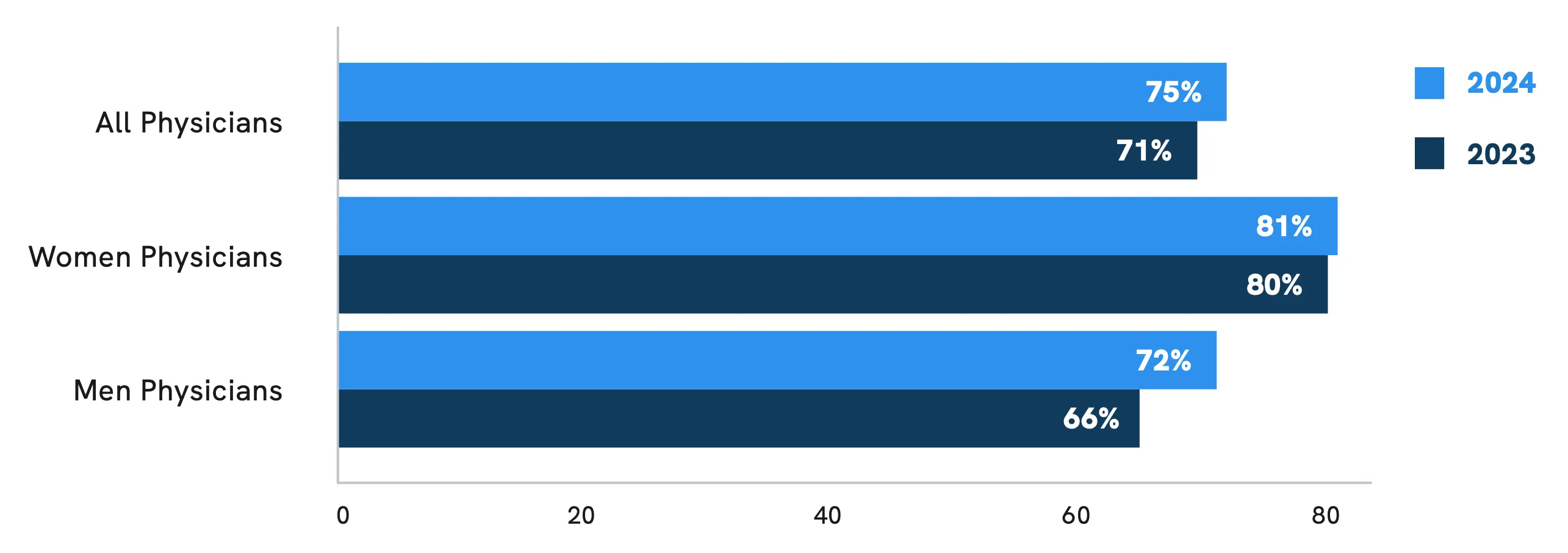
Increasing Number of Physicians Willing to Accept Lower Pay for More Autonomy, Work-Life Balance
Rather than negotiate a raise in salary, many physicians might be willing to accept lower compensation for more autonomy or work-life balance. In a Doximity poll of over 2,500 physicians, 75% reported they would be willing to accept, or have already accepted, lower compensation for more autonomy or work-life balance, up from 71% last year.
Consistent with last year’s findings, a greater proportion of women than men physicians said they have already accepted, or would be willing to accept, lower pay to achieve more autonomy or work-life balance (81% of women respondents, compared with 72% of men). However, this trend appears to have gained favor among men physicians over the last year.
Percentage of Physicians Who Have Accepted, or Would Accept, Lower Compensation for More Autonomy or Work-Life Balance
Impact of Overwork on Physician Career Plans
Majority of Physicians Surveyed Overworked and Considering an Employment Change
According to the U.S. Surgeon General, even before the COVID-19 pandemic, 54% of physicians and nurses were experiencing burnout.4 In a recent Doximity poll of over 2,600 physicians, four out of five physicians (81%) reported they are overworked, with nearly three out of five (59%) considering an employment change. These figures are down slightly from 86% of physicians who reported feeling overworked in 2022, but still a substantial increase from 73% in 2021.
How has your clinical workload altered your career plans?
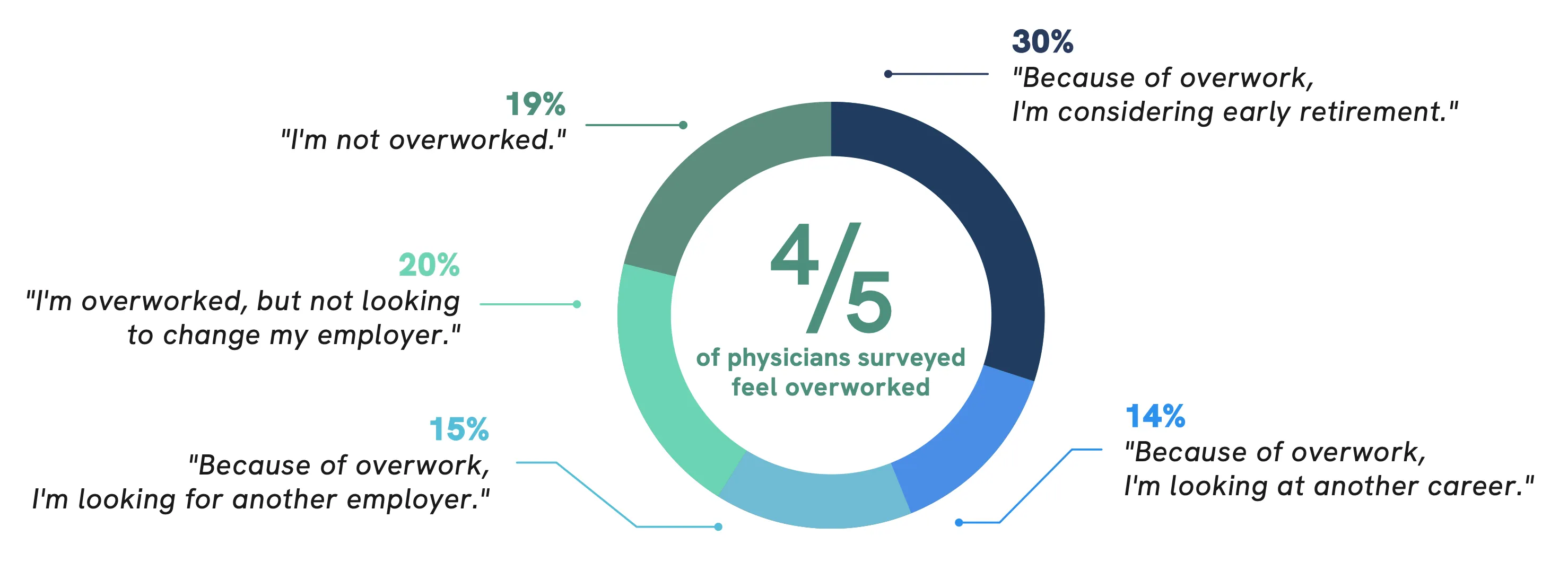
*Due to rounding, numbers may not sum to 100%.
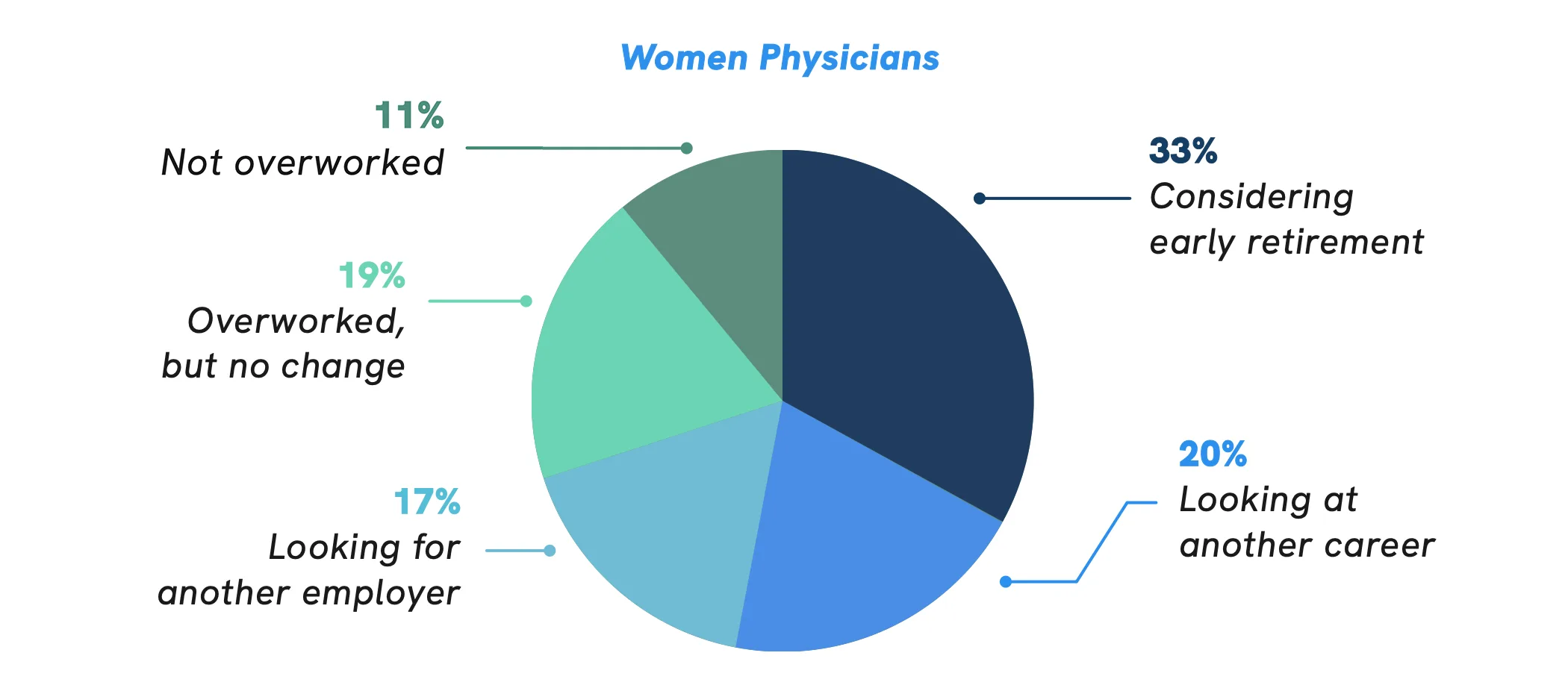
Impact of Overwork on Women and Early-Career Physicians
Women and Younger Physicians Report Highest Rates of Overwork
Consistent with prior years’ findings, feelings of overwork continue to be more prevalent in women physicians. Among women physicians surveyed, 89% reported they are overworked, compared with 77% of men physicians, 82% of women NPs and PAs, and 78% of men NPs and PAs. Women physicians are also more likely to report exploring a career change, with 70% considering early retirement, another career, or another employer, compared to 55% of men physicians.
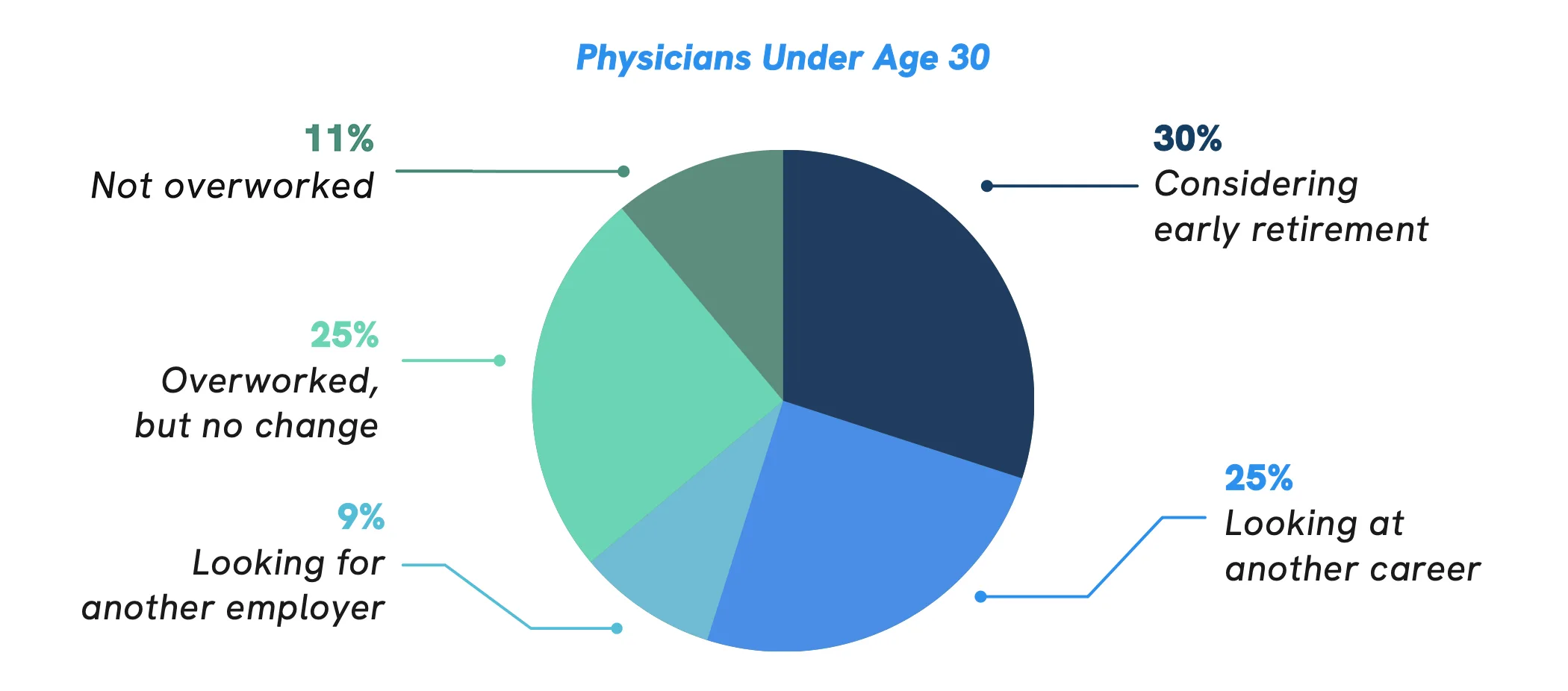
Overwork also appears to be more prevalent in younger physicians, with 89% of physicians age 29 and under reporting they feel overworked. Physicians 29 and under are likely trainees, who are often tasked with the longest hours for the least pay. Many of these physicians also started their training or attending careers at the peak of the pandemic, which likely contributed to their overall stress and workload. 5 As a result, 55% of physicians in this age group are already considering early retirement or looking at other career options.
Women physicians often face a third and fourth shift, balancing the rigorous demands of their medical careers with disproportionate expectations at home. Many of these expectations, both at work and at home, are uncompensated, unpromotable, and unappreciated.
How has your clinical workload altered your career plans?
Opportunities to Improve Physician Overwork, Burnout
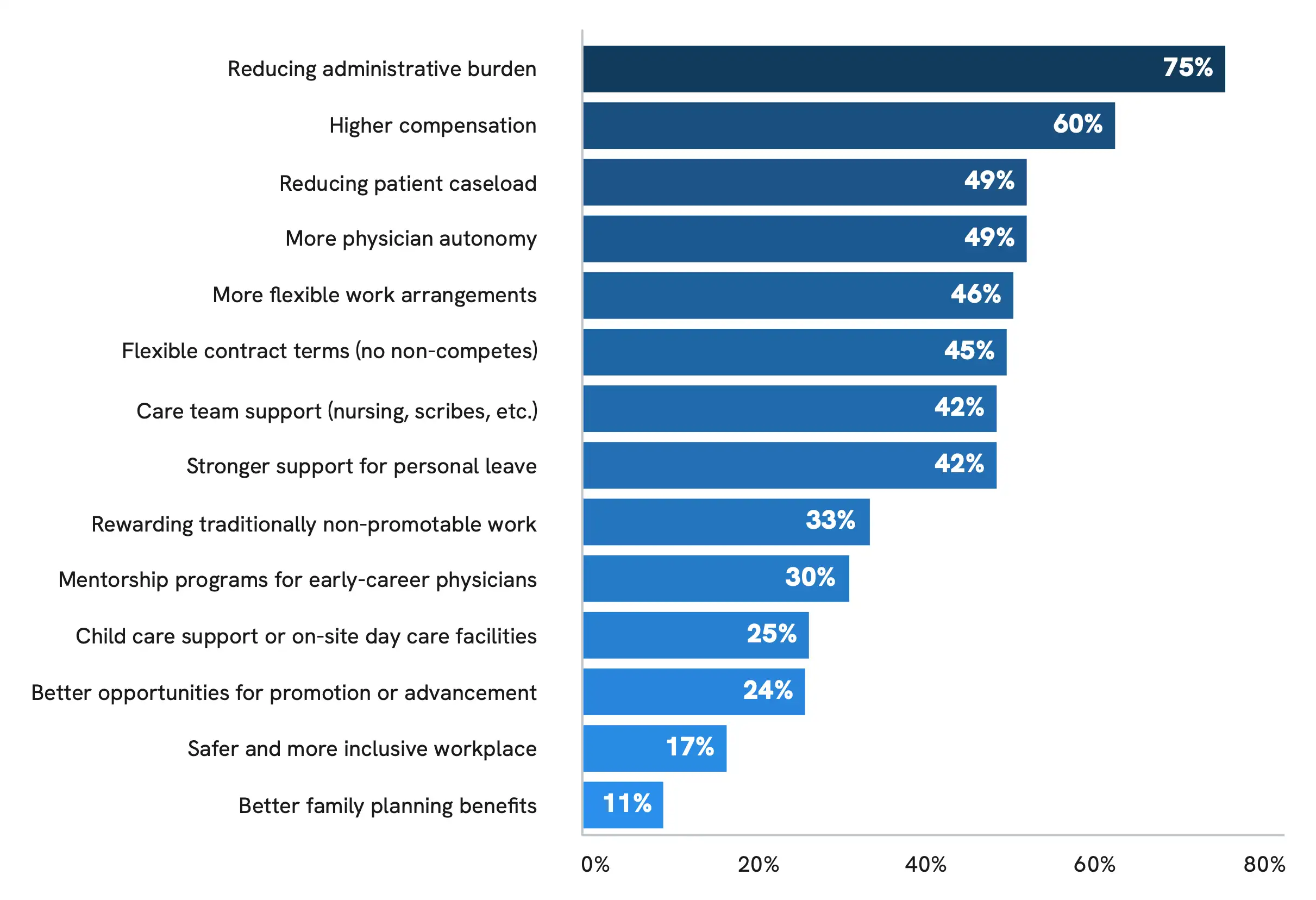
Reducing Administrative Burden Critical to Addressing Physician Burnout
While a number of factors are contributing to the burnout crisis, administrative burden remains one of the most significant drains on physician time and energy. Research shows that for every hour of direct patient care, physicians spend nearly two additional hours on EHR and desk work during the clinical day, with another one to two hours on clerical work each night.6
Among all physicians surveyed, 75% said that reducing administrative burden could meaningfully improve physician overwork and burnout. This response was even more prevalent than increasing physician compensation and reducing patient caseloads. Notably, primary care physicians, who serve on the frontlines of patient care and tend to be on the lower end of physician compensation, also favored reducing administrative burden (80% of primary care physicians) even more than higher pay (62%) and reduced patient caseloads (60%).
Another welcome change among women physicians, in particular, is more flexible work arrangements. Over 57% of women physicians said increased flexibility could meaningfully improve overwork and burnout, compared to 36% of men physicians. One potential explanation for this finding is that women often take on more home and family-related responsibilities, including child care. When asked about child care support as an employment benefit, such as onsite services, 60% of women physicians said availability has been insufficient. In comparison, 51% of men physicians said child care support as an employment benefit was not important to them.
In your opinion, what changes could meaningfully improve physician overwork and burnout?
Physician Shortage


Physician Shortage Overview and Impact
Majority of Physicians Report Moderate or Severe Impact of Shortage
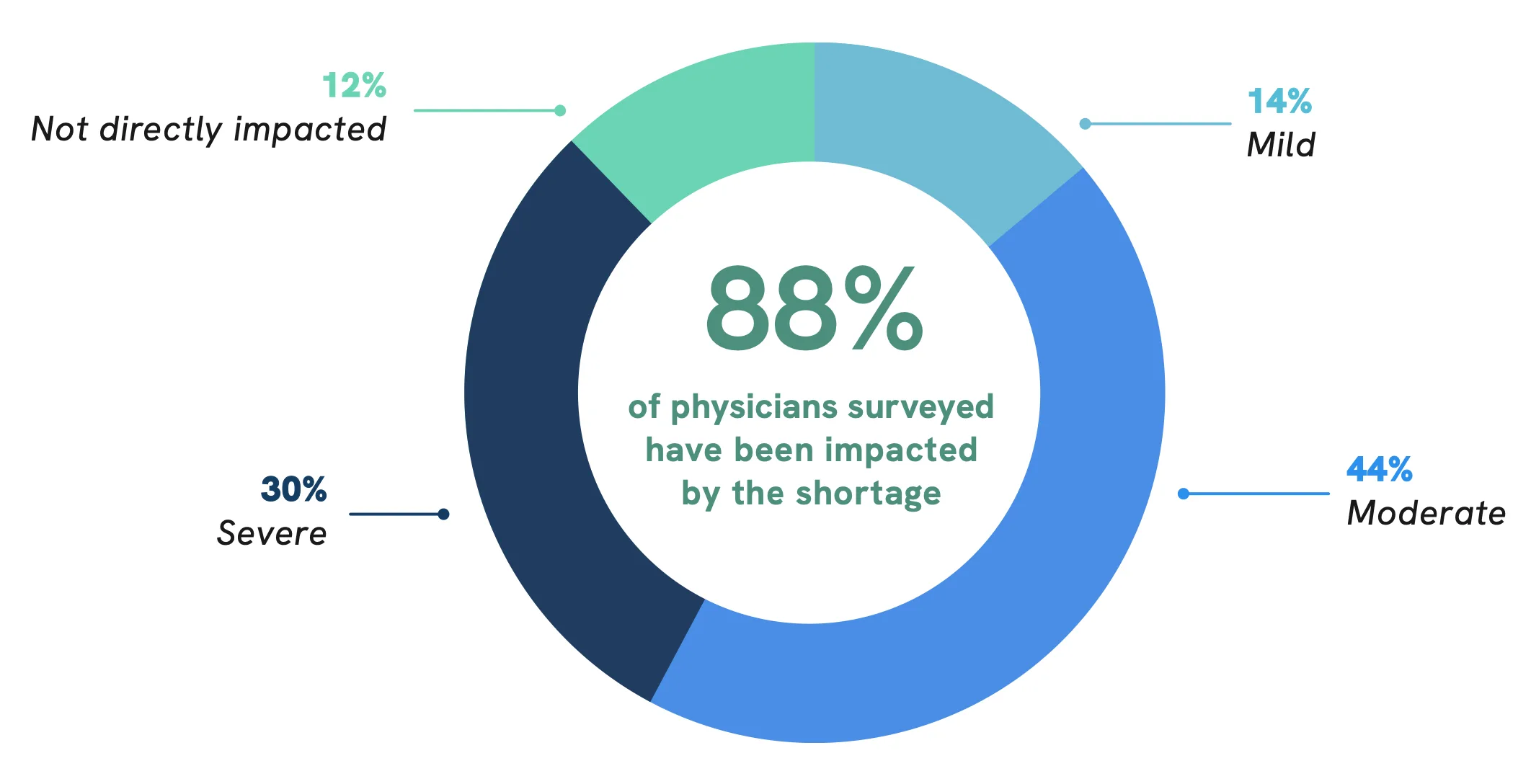
A report published by the Association of American Medical Colleges (AAMC) projects that the U.S. will face a physician shortage of up to 86,000 physicians by 2036.7 While this shortage is smaller than AAMC’s 2021 projections (up to 124,000 physicians by 2034), the physician shortage remains a critical patient access issue.
To learn more about the current state of the physician shortage and its impact on both patient care and physician well-being, Doximity conducted a survey of more than 1,100 U.S. physicians in February and March 2024. Among all physicians surveyed, 88% said that their clinical practice has been impacted by the physician shortage, and 74% described the shortage as “moderate” or “severe.” Only 12% of all physicians surveyed said they have not been impacted by the shortage.
How would you describe the impact of the physician shortage in your clinical practice?
Impact of Physician Shortage by Practice Setting
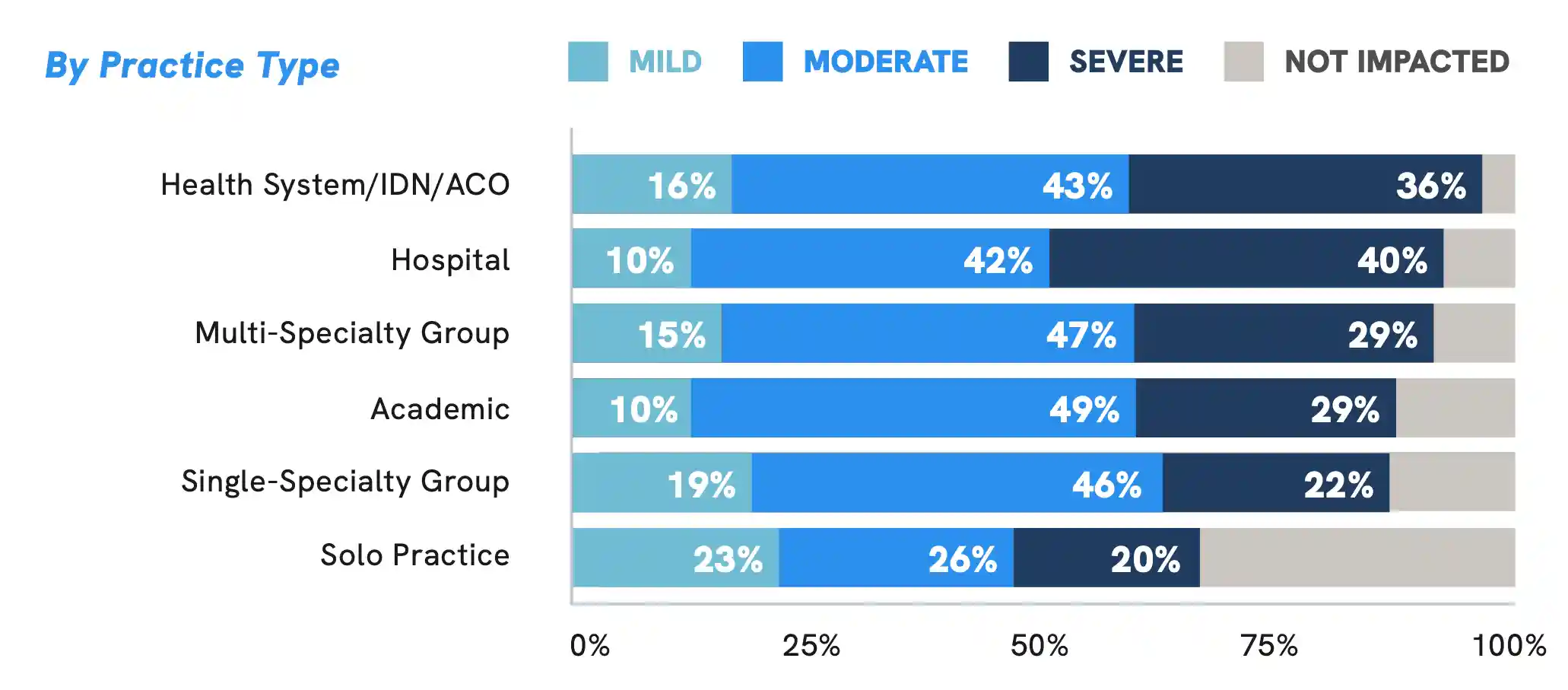
Physicians Across All Practice Settings Have Been Impacted by Shortage
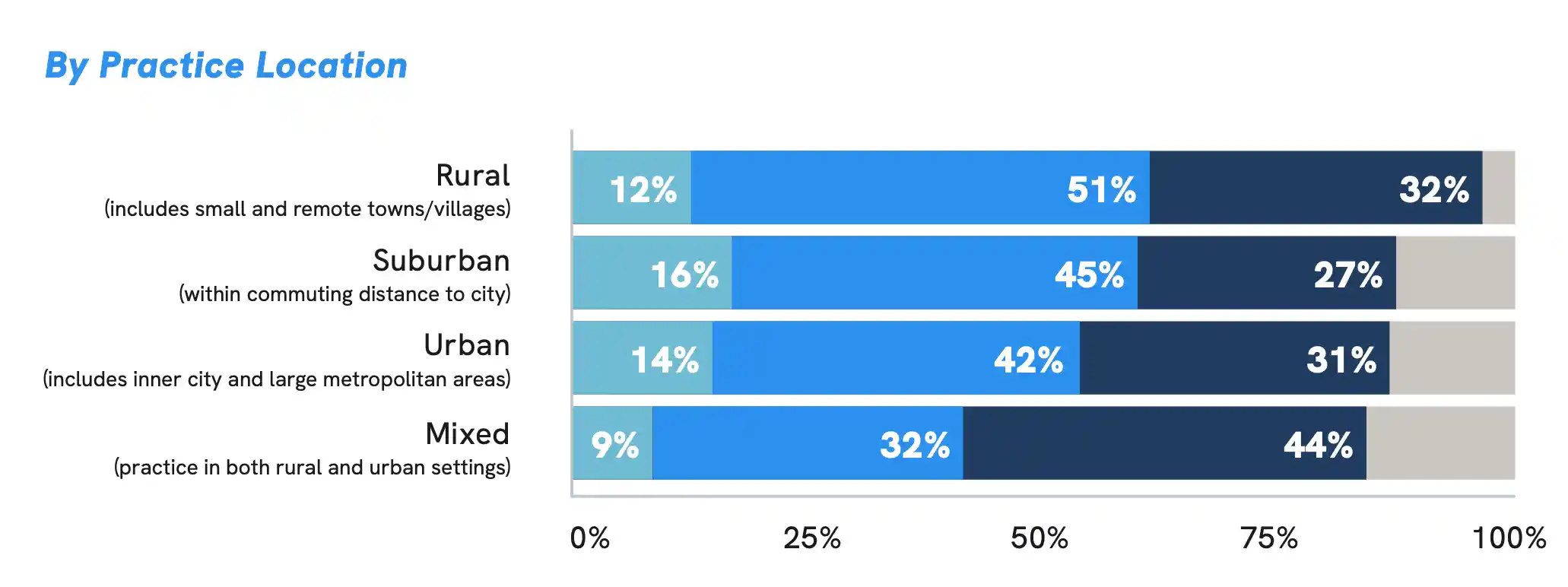
Across all practice settings studied, a substantial portion of physicians reported the impact of the shortage is moderate or severe in their clinical practice. While the physician shortage issue appears to be widespread, physicians working at larger health organizations and in either rural or a combination of urban and rural settings appear to be among the most heavily impacted.

How would you describe the impact of the physician shortage in your clinical practice?
Impact of Shortage on Physician Well-Being
Half of Physicians Are Having Thoughts About Leaving Clinical Practice Due to Shortage
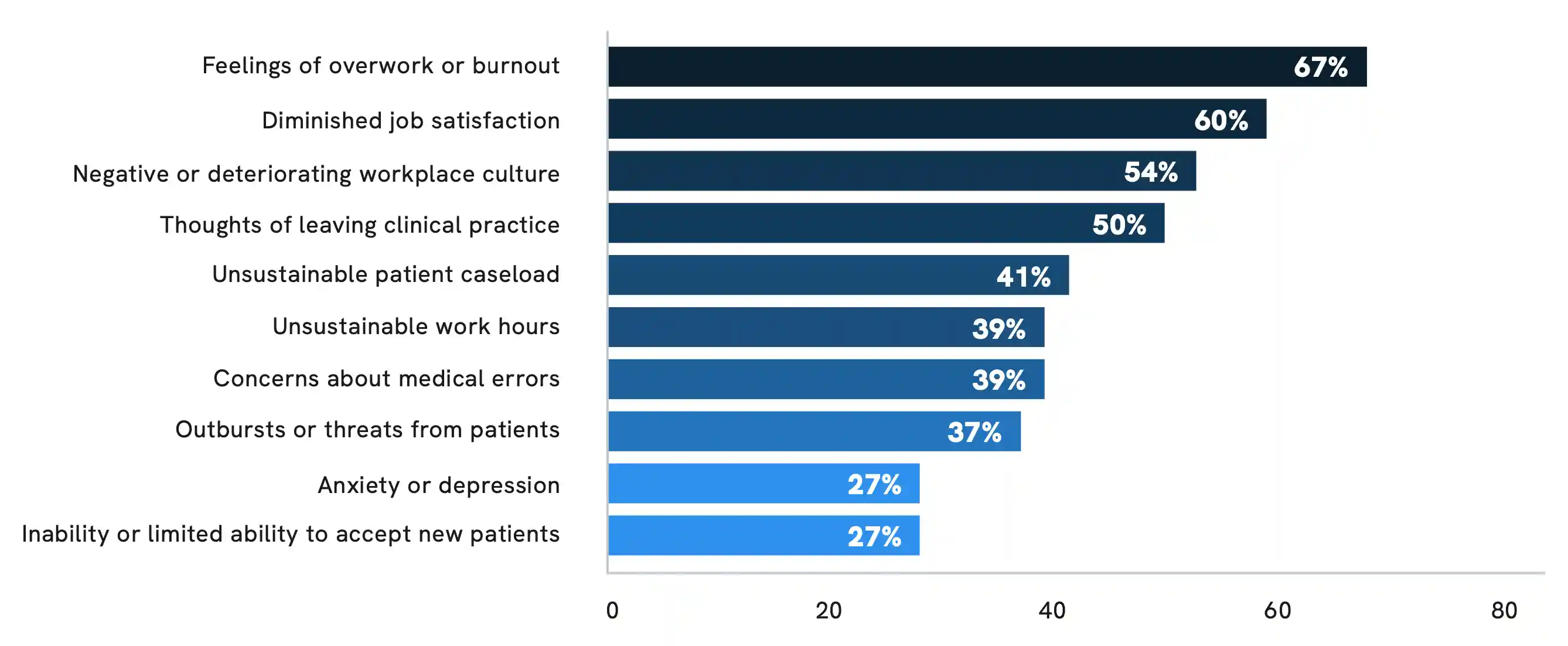
As a direct result of the physician shortage, the majority of physicians surveyed said they have experienced overwork or burnout (67%), diminished job satisfaction (60%), and deteriorating workplace culture (54%). A substantial portion of physicians have also faced unsustainable patient caseloads (41%) and work hours (39%), concerns about medical errors (39%), outbursts or threats from patients (37%), and even anxiety or depression (27%). With such significant consequences, half of all physicians surveyed are having thoughts about leaving clinical practice altogether.
Which of the following have you personally experienced as a result of the physician shortage?
Impact on Patient Access
Physician Shortage Poses Significant Consequences for Patients
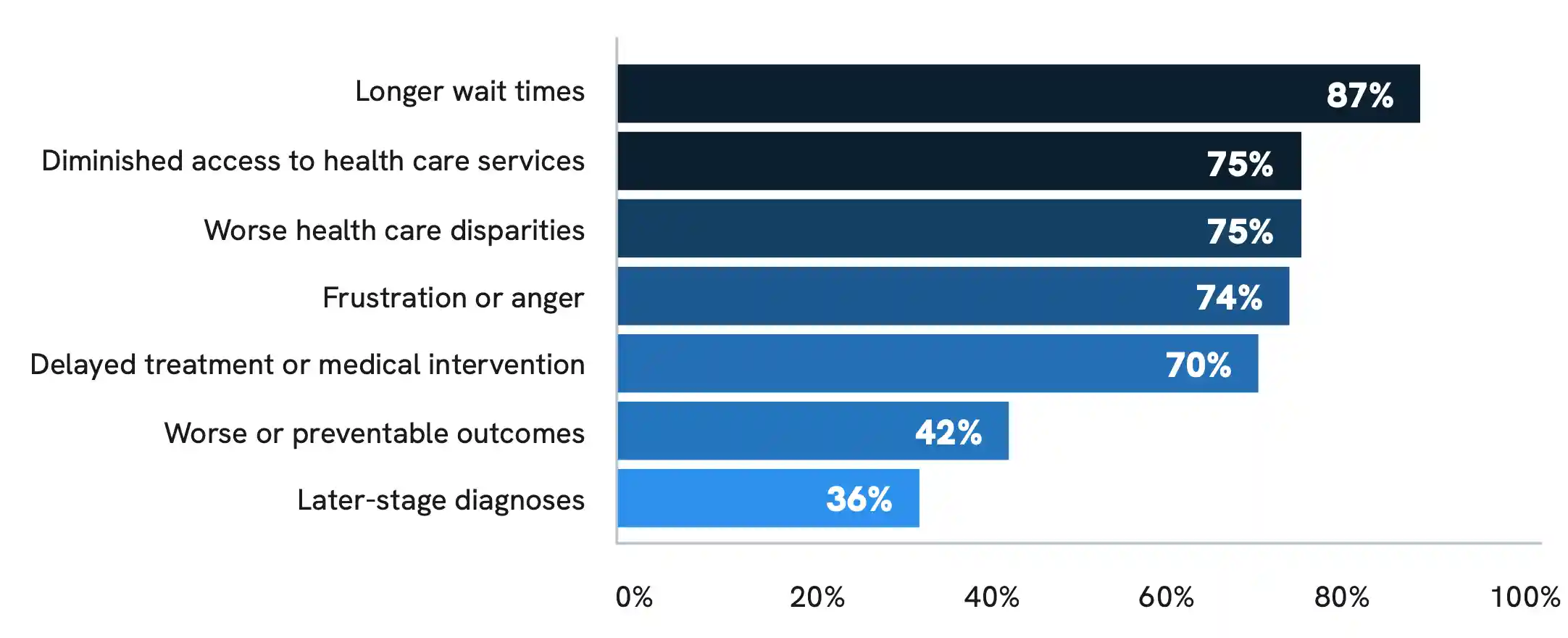
Consequences associated with the physician shortage are not limited to physicians and medical professionals. The majority of all physicians surveyed believe that the shortage has negatively impacted patients, leading to longer wait times (87%), diminished access to care (75%), worse health care disparities (75%), frustration or anger (74%), and delayed treatment (70%). Many physicians also believe the shortage has contributed to worse or preventable outcomes (42%) and later-stage diagnosis (36%) in some patients.
In a related Doximity poll of nearly 3,000 U.S. physicians, 93% said they have experienced clinical staffing shortages, and 82% said it has negatively impacted patient care.
From your perspective, which of the following have patients experienced as a result of the physician shortage?
Caring for a Growing, Aging Population
86% of Physicians Concerned About Adequate Care for Aging U.S. Population
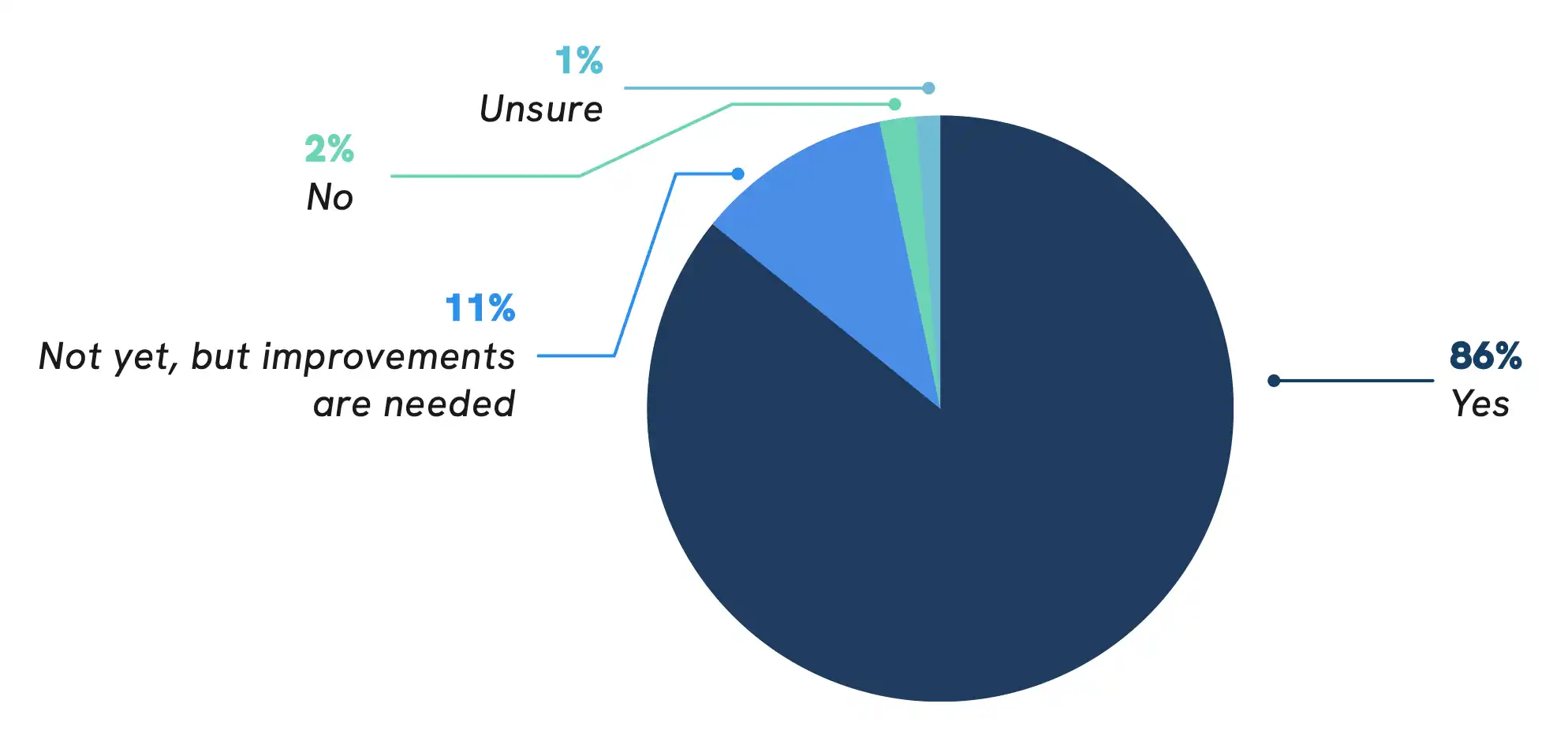
The physician shortage issue is further complicated by an expanding and aging U.S. population that will require more care over time. According to the Association of American Medical Colleges (AAMC), the U.S. population is projected to grow by 8.4% from 2021 to 2036. During this same period, the portion of the population aged 65 and older is expected to grow 34.1%, and the population aged 75 and older is projected to grow 54.7%.7
Among all physicians surveyed, 86% said they are concerned about U.S. health care’s ability to care for an aging population, and this number is even higher among primary care physicians (91%).
Are you concerned about U.S. health care’s ability to care for an aging population?
Factors Contributing to the Physician Shortage
Administrative Burden Among Top Drivers of Shortage Issue
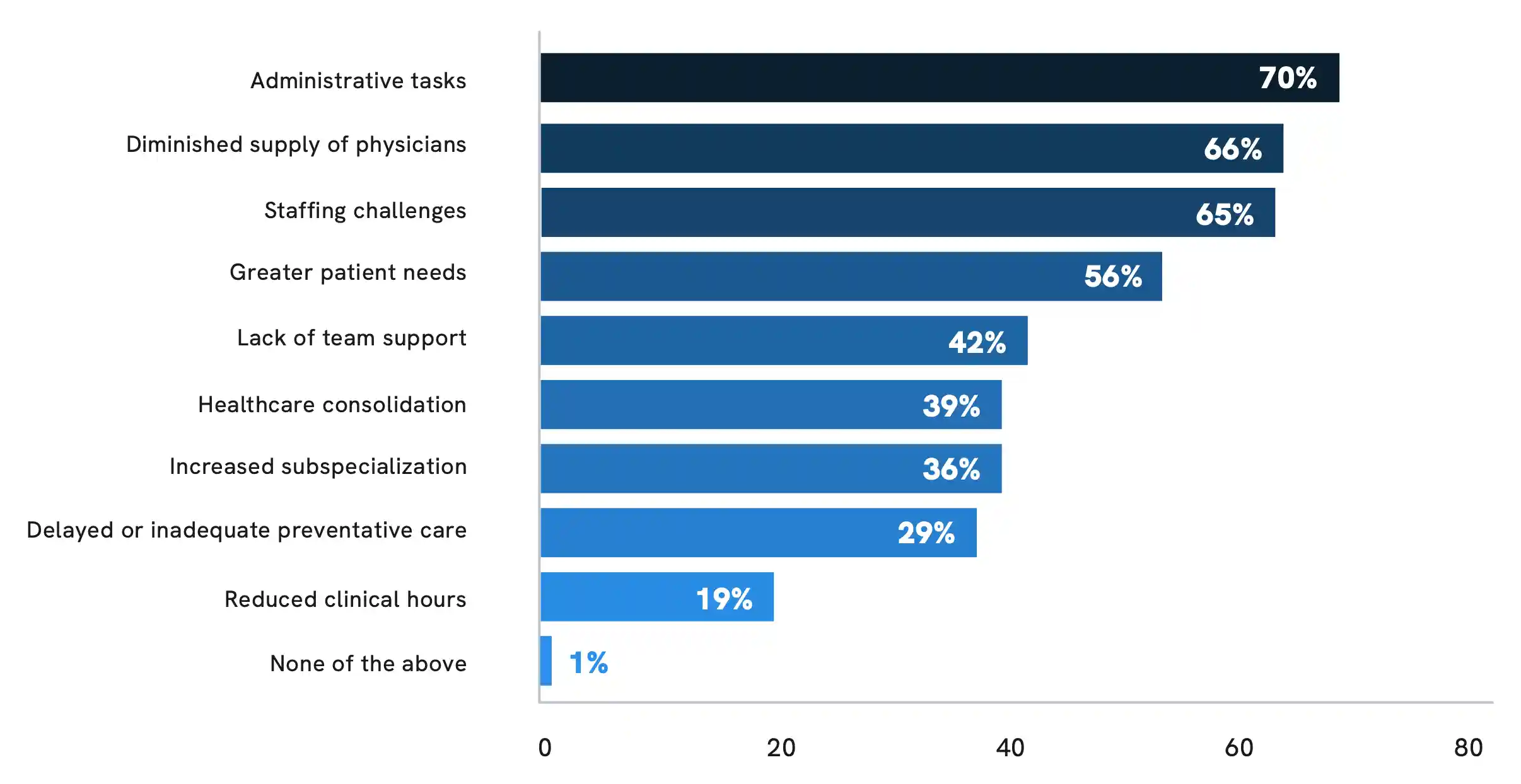
Beyond a growing and aging U.S. population, physicians cited a number of factors contributing to the physician shortage, led above all by administrative burden (70% of physicians surveyed). Other key factors contributing to the shortage include a diminished supply of physicians (66%), staffing challenges (65%), greater patient needs (56%), lack of care team support (42%), and health care consolidation (39%).
In your experience, which factors are directly contributing to the physician shortage?
Strategies to Alleviate the Physician Shortage
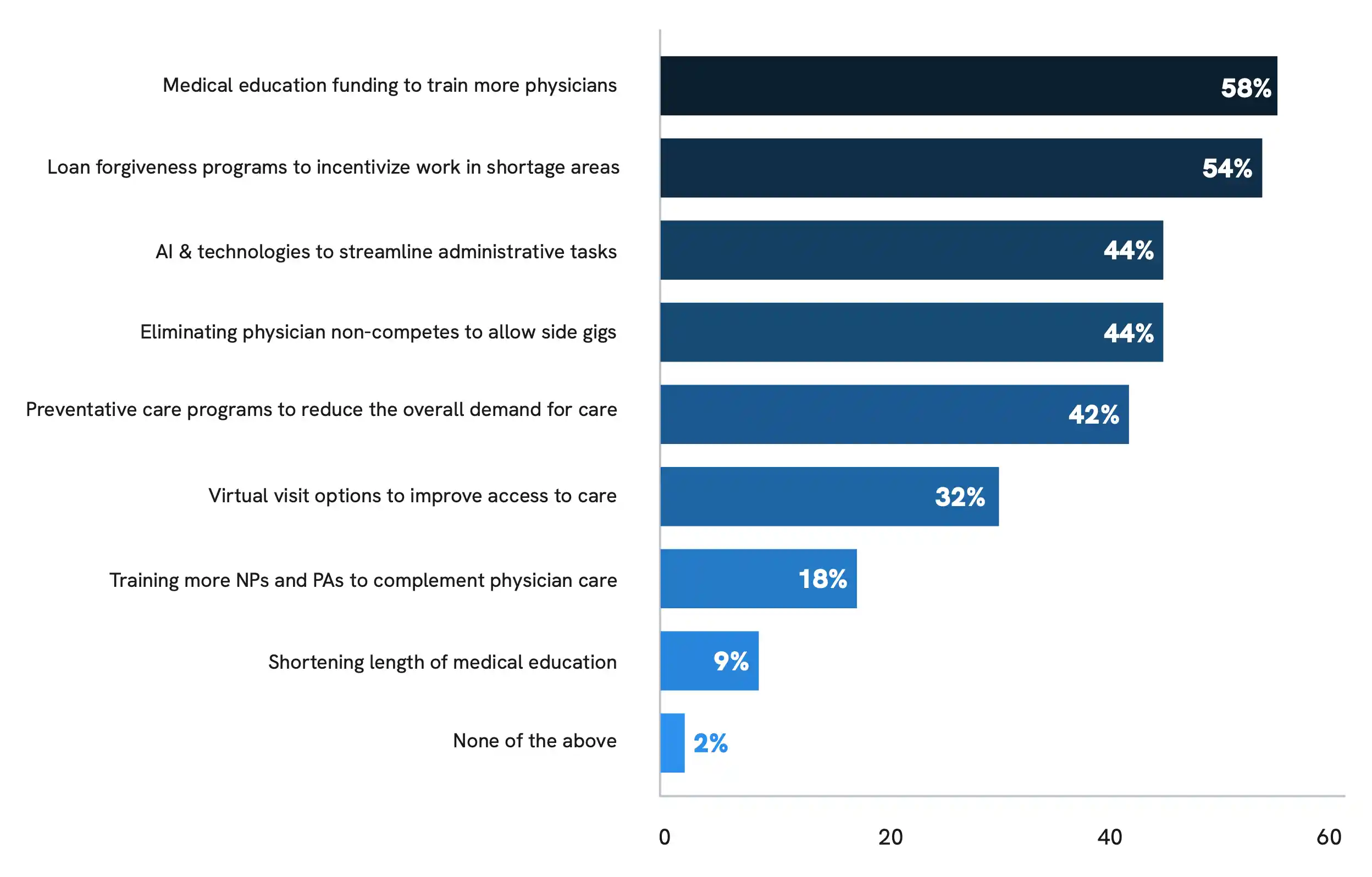
Top Strategies Include More Funding, Loan Forgiveness Programs, and AI/Technology
Despite the gravity of the physician shortage issue, only 3% of physicians surveyed said they feel adequately supported by health care institutions and policymakers to address the challenges posed by the shortage. While reducing administrative burden appears to be critical, respondents also identified many systems-level strategies that could help alleviate the impact of the shortage. These strategies include increasing medical education funding to train more physicians, implementing loan forgiveness programs to incentivize work in underserved areas, leveraging AI and technologies to streamline administrative tasks, and expanding virtual visit options to enhance patient access to care.

Which types of systems-level strategies could help alleviate the impact of the physician shortage?
Methodology & Sources


Methodology
This study by Doximity was drawn from over 33,000 physician compensation surveys completed between January and December 2023, with data from approximately 150,000 compensation surveys over the last five years. Each survey was completed by full-time U.S. physicians who practice at least 40 hours per week. Responses were mapped across metropolitan statistical areas, and 50 of the top represented MSAs were included in the analysis.
To control for differences in specialty, geography, and other provider-specific factors, we estimated a multivariate regression with controls for provider specialty, metro area, and gender. We also controlled for how long each provider has practiced medicine and their self-reported average hours worked per week.
Cost of Living Adjustment
This analysis used the 2022 regional price parities of metro state areas published by the Bureau of Economic Analysis. The price parties are publicly available in the December 14, 2023 release on the BEA website.
Physician Career and Compensation Satisfaction Survey
Doximity conducted a survey of its physician membership via SurveyMonkey in February and March 2024 about their career and compensation satisfaction. This survey was completed by over 1,000 U.S. physicians across a broad range of medical specialties, including primary care, emergency medicine and critical care, and both surgical and non-surgical specialties. Survey participant demographics are not population-based. Therefore, findings may not be able to be extrapolated to the broader physician population.
Autonomy and Work-Life Balance Poll
Doximity’s findings are based on a poll run in the Doximity Newsfeed in April 2024. Over 2,500 U.S. physicians responded.
The poll asked the following question: “Would you be willing to accept lower compensation to achieve more autonomy or work-life balance?”
The poll offered the following five answer options:
- “Yes, and I have already done so.”
- “Yes, I would consider it.”
- “No, probably not.”
- “No, definitely not.”
- “Unsure.”
Physician Overwork Poll
Doximity’s findings are based on a poll run in the Doximity Newsfeed in October 2023. Over 4,000 clinicians, including more than 2,600 U.S. physicians, responded to the poll.
The poll asked the following question: “How has your clinical workload altered your career plans?”
The poll offered the following five answer options:
- “Because of overwork, I’m looking for another employer.”
- “Because of overwork, I’m looking at another career.”
- “Because of overwork, I’m considering early retirement.”
- “I am overworked, but not looking to change my employer.”
- “I am not overworked.”
Physician Shortage Survey Doximity conducted a survey of its physician membership via SurveyMonkey in February and March 2024 about the impact of the physician shortage issue on patient access and physician well-being. This survey was completed by over 1,100 U.S. physicians, actively serving in clinical practice, across a broad range of medical specialties, including primary care, emergency medicine and critical care, and both surgical and non-surgical specialties. Survey participant demographics are not population-based. Therefore, findings may not be able to be extrapolated to the broader physician population.
Clinical Staffing Shortages Poll
Doximity’s findings are based on a poll run in the Doximity Newsfeed in August and September 2023. Nearly 3,000 U.S. physicians responded to the poll.
The poll asked the following question: “Have you experienced clinical staff shortages?”
The poll offered the following four answer options:
- “Yes, and it has negatively impacted patient care”
- “Yes, but it hasn’t impacted patient care”
- “No, I haven’t noticed a shortage”
- “No, but I know colleagues who have”
References
- 1Medicare Physician Pay Fell 26% Since 2001. How Did We Get Here? American Medical Association.
- 2Consumer Prices Up 9.1 Percent Over the Year Ended June 2022, Largest Increase in 40 Years. U.S. Bureau of Labor Statistics.
- 3Whaley CM, Koo T, Arora VM, Ganguli I, Gross N, Jena AB. Female Physicians Earn An Estimated $2 Million Less Than Male Physicians Over A Simulated 40-Year Career. Health Affairs. 2021 Dec;40(12):1856-1864
- 4New Surgeon General Advisory Sounds Alarm on Health Worker Burnout and Resignation. U.S. Department of Health and Human Services.
- 5Burned out by COVID and 80-hour Workweeks, Resident Physicians Unionize. Fierce Healthcare.
- 6Sinsky C, Colligan L, Li L, Prgomet M, Reynolds S, Goeders L, Westbrook J, Tutty M, Blike G. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Annals Intern Medicine. 2016;165:753-760
- 7The Complexities of Physician Supply and Demand: Projections From 2021 to 2036. Association of American Medical Colleges.