Join to View Full Profile
20 Penn StHSF II, room S247Baltimore, MD 21230
Phone+1 410-706-4205
Fax+1 410-706-1639
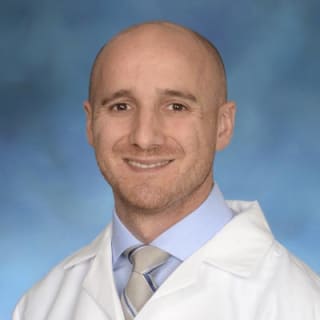
Dr. Faden is on Doximity
As a Doximity member you'll join over two million verified healthcare professionals in a private, secure network.
- Gain access to free telehealth tools, such as our “call shielding” and one-way patient texting.
- Connect with colleagues in the same hospital or clinic.
- Read the latest clinical news, personalized to your specialty.
Summary
- Dr. Alan Faden is a neurologist in Baltimore, MD and is affiliated with University of Maryland Medical Center. He received his medical degree from University of Chicago Division of the Biological Sciences The Pritzker School of Medicine and has been in practice 46 years. He has expertise in neurotrauma, neuroimmunology and molecular neuroscience. . He has more than 400 publications and over 43,000 citations.
Education & Training
 University of California (San Francisco)Residency, Neurology, 1972 - 1975
University of California (San Francisco)Residency, Neurology, 1972 - 1975 University of Pennsylvania Health SystemInternship, Internal Medicine, 1971 - 1972
University of Pennsylvania Health SystemInternship, Internal Medicine, 1971 - 1972 University of Chicago Division of the Biological Sciences The Pritzker School of MedicineClass of 1971
University of Chicago Division of the Biological Sciences The Pritzker School of MedicineClass of 1971
Certifications & Licensure
 CA State Medical License 1972 - Present
CA State Medical License 1972 - Present MD State Medical License 1976 - 2026
MD State Medical License 1976 - 2026 DC State Medical License 1991 - 2018
DC State Medical License 1991 - 2018 American Board of Psychiatry and Neurology Neurology
American Board of Psychiatry and Neurology Neurology
Awards, Honors, & Recognition
- Distinguished Service Award University of Chicago, 2001
- Exceptional Service Medal Uniformed Services University of the Health Sciences, 1984
- American Society for Clinical Investigation 1981
- Join now to see all
Publications & Presentations
PubMed
- Molecular Pathway Changes Associated with Different Post-Conditioning Exercise Interventions After Experimental TBI.James P Barrett, Taryn G Aubrecht, Aidan Smith, Maria Vaida, Rebecca J Henry
Journal of Neurotrauma. 2024-08-21 - 1 citationsSpinal cord injury disrupts plasma extracellular vesicles cargoes leading to neuroinflammation in the brain and neurological dysfunction in aged male mice.Zhuofan Lei, Balaji Krishnamachary, Niaz Z Khan, Yuanyuan Ji, Yun Li
Brain, Behavior, and Immunity. 2024-08-01 - 1 citationsOld age alters inflammation and autophagy signaling in the brain, leading to exacerbated neurological outcomes after spinal cord injury in male mice.Zhuofan Lei, Rodney M Ritzel, Yun Li, Hui Li, Alan I Faden
Brain, Behavior, and Immunity. 2024-08-01
Press Mentions
 Depletion and Repopulation of Microglia Could Be a Future Therapy for TBIFebruary 26th, 2020
Depletion and Repopulation of Microglia Could Be a Future Therapy for TBIFebruary 26th, 2020 UM School of Medicine's Shock Trauma and Anesthesiology Research (STAR) Center Announces Leadership TransitionJanuary 27th, 2020
UM School of Medicine's Shock Trauma and Anesthesiology Research (STAR) Center Announces Leadership TransitionJanuary 27th, 2020 Microbleeds After Head Trauma Lead to Worse Neurological OutcomesNovember 21st, 2019
Microbleeds After Head Trauma Lead to Worse Neurological OutcomesNovember 21st, 2019- Join now to see all
Grant Support
- Bidirectional Brain-Gut interactions, chronic neuroinflammation and neurodegeneration after traumatic brain injuryUNIVERSITY OF MARYLAND BALTIMORE2022–2027
- Microglial NOX2 drive pro-inflammatory responses and neurodegeneration after traumatic brain injury.National Institute of Neurological Disorders and Stroke2022–2027
- Bidirectional Brain-Gut interactions Recovery, chronic neuroinflammation and neurodegeneration after Traumatic Brain Injury.National Institute of Neurological Disorders and Stroke2022–2027
- Reprogramming Microglial Epigenetic Pathways to Promote Cognitive Recovery after Brain Trauma.UNIVERSITY OF MARYLAND BALTIMORE2019–2025
- Mechanism of Inflammatory Related Brain Dysfunction after Spinal Cord InjuryUNIVERSITY OF MARYLAND BALTIMORE2019–2025
- Dementia Following Spinal Cord Injury: Mechanism and Therapeutic TargetingNational Institue of Neurologicl Disorders and Stroke2019–2024
- Mechanism of Inflammatory Related Brain Dysfunction after Spinal Cord Injury.National Institute of Neurological Disorders and Stroke2019–2024
- Reprogramming Microglial Epigenetic Pathways to Promote Cognitive Recovery after Brain Trauma.National Institue of Neurological Disorders and Stroke2019–2024
- Spinal Mechanisms Underlying SCI-Induced Pain: Implications for Targeted Therapy.National Institute of Nursing Research2012–2023
- miR-711 regulation of neuronal cell death after traumatic brain injury.NIH2016–2022
- Effect of Hypobaria on Systemic Immune Function following Brain TraumaAir Foce2018–2021
- Mechanisms of Autophagy-Lysosomal Pathway in Traumatic Brain InjuryNIH2015–2021
- Role of miR-23a/27a in secondary injury after TBI.NIH2015–2021
- mGluR5 inhibits microglial activation and neuronal cell death after TBINIH1998–2021
- Biomarkers and Treatment of Hypobaria-Exacerbated TBIAir Force2016–2019
- Role of Cell Cycle Pathways after Traumatic Brain InjuryNIH2006–2018
- Center for the Genomics of PainNIH2012–2017
- Prolonged Hypobaria during Aeromedical Evacuation and the Effects on TBIAir Force2011–2014
- Mechanism and Modulation of Cell Death in Traumatic brain InjuryNIH2009–2014
- Cell Cycle Pathways And Spinal Cord InjuryNational Institute Of Neurological Disorders And Stroke2010–2011
- Combination Drug Treatment To Inhibit Multiple Cell Death Pathways After TBIEunice Kennedy Shriver National Institute Of Child Health &Human Development2009–2010
- Cell Cycle Pathways And Spinal Cord InjuryNational Institute Of Neurological Disorders And Stroke2007–2010
- Role Of Cell Cycle Pathways In Traumatic Brain InjuryNational Institute Of Neurological Disorders And Stroke2009
- Mglur5 Inhibits Microglial Activation And Neuronal Cell Death After TBINational Institute Of Neurological Disorders And Stroke2009
- Mechanisms And Modulation Of Cell Death In Traumatic Brain InjuryNational Institute Of Neurological Disorders And Stroke2009
- Role Of Cell Cycle Pathways In Traumatic Brain InjuryNational Institute Of Neurological Disorders And Stroke2006–2009
- Modulation Of Injury By Metabotropic Glutamate ReceptorsNational Institute Of Neurological Disorders And Stroke1999–2006
- Apoptosis Induced By Traumatic Brain InjuryNational Institute Of Neurological Disorders And Stroke1998–2005
- Core--Cellular Neuroscience FacilityEunice Kennedy Shriver National Institute Of Child Health &Human Development2001–2002
- Multipontential Drug Treatment Strategies In NeurotramaNational Institute Of Neurological Disorders And Stroke2000–2002
- Excitotoxins, Cellular Bioenergetics, And Brain InjuryNational Institute Of Neurological Disorders And Stroke1994
- Excitotoxins, Cellular Bioenergetics And Brain InjuryNational Institute Of Neurological Disorders And Stroke1991–1993
- Exitotoxins, Bioenergetics &Traumatic Brain InjuryNational Institute Of Neurological Disorders And Stroke1990–1991
- Opioids, Opiate Receptors And Spinal Cord InjuryNational Institute Of Neurological Disorders And Stroke1987–1989
Viewing the full profile is available to verified healthcare professionals only.
Find your profile and take control of your online presence: